- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences

Unconscious Bias Training That Works
- Francesca Gino
- Katherine Coffman

To become more diverse, equitable, and inclusive, many companies have turned to unconscious bias (UB) training. By raising awareness of the mental shortcuts that lead to snap judgments—often based on race and gender—about people’s talents or character, it strives to make hiring and promotion fairer and improve interactions with customers and among colleagues. But most UB training is ineffective, research shows. The problem is, increasing awareness is not enough—and can even backfire—because sending the message that bias is involuntary and widespread may make it seem unavoidable.
UB training that gets results, in contrast, teaches attendees to manage their biases, practice new behaviors, and track their progress. It gives them information that contradicts stereotypes and allows them to connect with colleagues whose experiences are different from theirs. And it’s not a onetime session; it entails a longer journey and structural organizational changes.
In this article the authors describe how rigorous UB programs at Microsoft, Starbucks, and other organizations help employees overcome denial and act on their awareness, develop the empathy that combats bias, diversify their networks, and commit to improvement.
Increasing awareness isn’t enough. Teach people to manage their biases, change their behavior, and track their progress.
Idea in Brief
The problem.
Conventional training to combat unconscious bias and make the workplace more diverse, equitable, and inclusive isn’t working.
This training aims to raise employees’ awareness of biases based on race or gender. But by also sending the message that such biases are involuntary and widespread, it can make people feel that they’re unavoidable.
The Solution
Companies must go beyond raising awareness and teach people to manage biases and change behavior. Firms should also collect data on diversity, employees’ perceptions, and training effectiveness; introduce behavioral “nudges”; and rethink policies.
Across the globe, in response to public outcry over racist incidents in the workplace and mounting evidence of the cost of employees’ feeling excluded, leaders are striving to make their companies more diverse, equitable, and inclusive. Unconscious bias training has played a major role in their efforts. UB training seeks to raise awareness of the mental shortcuts that lead to snap judgments—often based on race and gender—about people’s talents or character. Its goal is to reduce bias in attitudes and behaviors at work, from hiring and promotion decisions to interactions with customers and colleagues.
- Francesca Gino is a behavioral scientist and the Tandon Family Professor of Business Administration at Harvard Business School. She is the author of Rebel Talent and Sidetracked . francescagino
- KC Katherine Coffman is an associate professor of business administration at Harvard Business School. Her research focuses on how stereotypes affect beliefs and behavior.
Partner Center

What Is Unconscious Bias (And How You Can Defeat It)
Research-based strategies for how to identify and defeat unconscious bias..
Posted July 13, 2020 | Reviewed by Lybi Ma
- What Is the Unconscious
- Find a therapist near me

How do you defeat unconscious bias? First, you need to know what it is.
Unconscious bias (also known as implicit bias) refers to unconscious forms of discrimination and stereotyping based on race, gender , sexuality , ethnicity , ability, age, and so on. It differs from cognitive bias, which is a predictable pattern of mental errors that result in us misperceiving reality and, as a result, deviating away from the most likely way of reaching our goals .
In other words, from the perspective of what is best for us as individuals, falling for a cognitive bias always harms us by lowering our probability of getting what we want. Despite cognitive biases sometimes leading to discriminatory thinking and feeling patterns, these are two separate and distinct concepts.
Cognitive biases are common across humankind and relate to the particular wiring of our brains, while unconscious bias relates to perceptions between different groups and are specific for the society in which we live. For example, I bet you don’t care or even think about whether someone is a noble or a commoner, yet that distinction was fundamentally important a few centuries ago across Europe. To take another example – a geographic instead of one across time – most people in the US don’t have strong feelings about Sunni vs. Shiite Muslims, yet this distinction is incredibly meaningful in many parts of the world.
Black Americans suffer from police harassment and violence at a much higher rate than white people, people do try to defend the police by claiming that black people are more violent and likely to break the law than whites. They thus attribute police harassment to the internal characteristics of black people (implying that it is deserved), not to the external context of police behavior.
In reality, research shows that black people are harassed and harmed by police at a much higher rate for the same kind of activity. A white person walking by a cop, for example, is statistically much less likely to be stopped and frisked than a black one. At the other end of things, a white person resisting arrest is much less likely to be violently beaten than a black one. In other words, statistics show that the higher rate of harassment and violence against black Americans by police is due to the prejudice of the police officers, at least to a large extent.
However, this discrimination is not necessarily intentional. Sometimes, it indeed is deliberate, with white police officers consciously believing that black Americans deserve much more scrutiny than whites. At other times, the discriminatory behavior results from unconscious, implicit thought processes that the police officer would not consciously endorse.
Interestingly, research shows that many black police officers have an unconscious prejudice against other black people, perceiving them in a more negative light than white people when evaluating potential suspects. This unconscious bias carried by many, not all, black police officers helps show that such prejudices come – at least to a significant extent – from internal cultures within police departments, rather than pre-existing racist attitudes before someone joins a police department.
Such cultures are perpetuated by internal norms, policies, and training procedures, and any police department wishing to address unconscious bias needs to address internal culture first and foremost, rather than attributing racism to individual officers. In other words, instead of saying it’s a few bad apples in a barrel of overall good ones, the key is recognizing that implicit bias is a systemic issue, and the structure and joints of the barrel need to be fixed.
The crucial thing to highlight is that there is no shame or blame in implicit bias, as it’s not stemming from any fault in the individual. This no-shame approach decreases the fight, freeze, or flight defensive response among reluctant people, helping them hear and accept the issue.
With these additional statistics and discussion of implicit bias, the issue is generally settled. Still, from their subsequent behavior, it’s clear that some people don’t immediately internalize this evidence. It’s much more comforting for them to feel that police officers are right and anyone targeted by police deserves it; in turn, they are highly reluctant to accept the need to focus more efforts and energy on protecting black Americans from police violence, due to the structural challenges facing these groups.

The issue of unconscious bias doesn’t match their intuitions and thus they reject this concept, despite extensive and strong evidence for its pervasive role in policing. It takes a series of subsequent follow-up conversations and interventions to move the needle.
This example of how to fight unconscious bias illustrates broader patterns you need to follow to address such problems to address unconscious bias to make the best people decisions. After all, our gut reactions lead us to make poor judgment choices, when we simply follow our intuitions.
1) Instead, you need to start by learning about the kind of problems that result from unconscious bias yourself, so that you know what you’re trying to address.
2) Then, you need to convey to people who you want to influence, such as your employees or any other group or even yourself, that there should be no shame or guilt in acknowledging our instincts.
3) Next, you need to convey the dangers associated with following their intuitions, to build up an emotional investment into changing behaviors.
4) Then, you need to convey the right mental habits that will help them make the best choices.
It takes a long-term commitment and constant discipline and efforts to overcome unconscious bias.
Originally Published at Disaster Avoidance Experts on June 23, 2020.
Tsipursky, G. (2019). Never Go With Your Gut: How Pioneering Leaders Make the Best Decisions and Avoid Business Disasters. Newburyport, MA: Career Press.

Gleb Tsipursky, Ph.D. , is on the editorial board of the journal Behavior and Social Issues. He is in private practice.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- Research bias
- What Is Unconscious Bias? | Definition & Examples
What Is Unconscious Bias? | Definition & Examples
Published on February 27, 2023 by Kassiani Nikolopoulou and Tegan George. Revised on August 9, 2024.
Unconscious bias refers to the automatic associations and reactions that arise when we encounter a person or group. Instead of maintaining neutrality, we tend to associate positive or negative stereotypes with certain groups and let these biases influence our behavior towards them.
Unconscious bias can lead to discriminatory behavior in healthcare, the workplace, educational settings, and beyond.
Table of contents
What is unconscious bias, what causes unconscious bias, unconscious vs. explicit bias, unconscious bias examples, how to reduce unconscious bias, other types of research bias, frequently asked questions about unconscious bias.
Unconscious bias is an implicit preference for (or aversion towards) a particular person or entity. These feelings can be either positive or negative, but they cause us to act unfairly towards others. This can manifest as affinity bias , or the tendency to favor people who are similar to us, but any identity-based aspect (e.g., age, gender identity, socioeconomic background, etc.) can be the target of unconscious bias.
We are, by definition, unaware of biases that affect our decisions and judgments: this is why they are called unconscious. For example, when most people hear the word “nurse,” they are more likely to picture a female, even if they don’t consciously believe that only women can be nurses. Because unconscious bias operates below our awareness, it can be challenging to acknowledge and manage.
There are several factors at play within our unconscious biases:
- Brain categorization . Humans have a natural tendency to assign everything into a relevant category. This happens unconsciously, but this categorizing also leads us to assign a positive or negative association to each category. Categories allow our brains to know what to do or how to behave, but classifications often cause us to overgeneralize.
- We rely on heuristics. We often rely on “automatic” information processing to go through our day, involving little conscious thought. These mental shortcuts allow us to exert little mental effort in our everyday lives, and make swift judgments when needed.
- Social and cultural dynamics. Our upbringing and social environment, as well as any direct and indirect experiences with members of various social groups, imprint on us. These shape our perceptions, both consciously and subconsciously.
Both unconscious and explicit bias involve judging others based on our assumptions rather than objective facts. However, the two are actually quite different.
- Unconscious bias occurs when we have an inclination for or against a person or group that emerges automatically .
- Explicit bias includes positive or negative attitudes that we are fully aware of and openly express. These attitudes form part of our worldview.
Despite their differences, unconscious bias can be just as problematic as explicit bias. Both can lead to discriminatory behavior.
Unconscious bias can lead to discriminatory behavior when it comes to hiring a diverse workforce.
Both positive and negative unconscious beliefs operate outside our awareness and can lead to structural and systemic inequalities. If we want to reduce it, we must first become conscious of it. The following strategies can help:
- Taking the Harvard Implicit Bias Association Test (IAT) can help you realize that everyone, including you, has implicit or unconscious biases. Recognising them for what they are increases the likelihood that next time you won’t let these hidden biases affect your behaviour.
- Seek out positive intergroup contact. Unconscious bias towards a particular group can be reduced through interaction with members of that group. For example, you can make it a point to engage in activities that include individuals from diverse backgrounds.
- Counter-stereotyping. Exposure to information that defies persistent stereotypes about certain groups, such as images of male nurses, can counter gender-based stereotypes.
- Unconscious bias training. Although raising awareness is important, it’s not sufficient to overcome unconscious biases. The most successful training programs are ones that allow individuals to discover their biases in a non-confrontational manner, helping them seek out the tools to help reduce and manage these biases.
Cognitive bias
- Confirmation bias
- Baader–Meinhof phenomenon
- Availability heuristic
- Halo effect
- Framing effect
- Optimism bias
- Negativity bias
- Affect heuristic
- Representativeness heuristic
- Anchoring heuristic
- Primacy bias
Selection bias
- Sampling bias
- Ascertainment bias
- Attrition bias
- Self-selection bias
- Survivorship bias
- Nonresponse bias
- Undercoverage bias
- Hawthorne effect
- Observer bias
- Omitted variable bias
- Publication bias
- Pygmalion effect
- Recall bias
- Social desirability bias
- Placebo effect
- Actor-observer bias
- Ceiling effect
- Ecological fallacy
- Affinity bias
Implicit bias refers to attitudes that affect our understanding, actions, and decisions in an unconscious manner. These attitudes can be either positive or negative. Affinity bias , or the tendency to gravitate towards people who are similar to us, is a type of implicit or unconscious bias.
Similarity bias or affinity bias is a type of unconscious bias. It occurs when we show preference for people who are similar to us (i.e., people with whom we share a common attribute, such as physical appearance, hobbies, or educational background).
The opposite of explicit bias is implicit bias (or unconscious bias). This refers to all the subconscious evaluations we have formed about a certain group. Implicit bias can influence our interactions with members of this group without us realizing.
Demand characteristics are a type of extraneous variable that can affect the outcomes of the study. They can invalidate studies by providing an alternative explanation for the results.
These cues may nudge participants to consciously or unconsciously change their responses, and they pose a threat to both internal and external validity . You can’t be sure that your independent variable manipulation worked, or that your findings can be applied to other people or settings.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Nikolopoulou, K. & George, T. (2024, August 09). What Is Unconscious Bias? | Definition & Examples. Scribbr. Retrieved September 16, 2024, from https://www.scribbr.com/research-bias/unconscious-bias/
Is this article helpful?

Kassiani Nikolopoulou
Other students also liked, what is implicit bias | definition & examples, what is explicit bias | definition & examples, what is affinity bias | definition & examples.
- Skip to main content
- Keyboard shortcuts for audio player

- LISTEN & FOLLOW
- Apple Podcasts
- Amazon Music
- Amazon Alexa
Your support helps make our show possible and unlocks access to our sponsor-free feed.
Understanding Unconscious Bias

The human brain sometimes takes cognitive shortcuts to help make decisions, shortcuts that can lead to implicit or unconscious bias. Damien Meyer/AFP via Getty Images hide caption
The human brain sometimes takes cognitive shortcuts to help make decisions, shortcuts that can lead to implicit or unconscious bias.
The human brain can process 11 million bits of information every second. But our conscious minds can handle only 40 to 50 bits of information a second. So our brains sometimes take cognitive shortcuts that can lead to unconscious or implicit bias, with serious consequences for how we perceive and act toward other people.
Where does unconscious bias come from? How does it work in the brain and ultimately impact society?
Short Wave reporter Emily Kwong speaks with behavioral and data scientist Pragya Agarwal , author of Sway: Unravelling Unconscious Bias .
Email the show at [email protected] .
Buy Featured Book
Your purchase helps support NPR programming. How?
- Independent Bookstores
This episode was produced by Rebecca Ramirez, fact-checked by Berly McCoy and edited by Viet Le.
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

‘Could I really cut it?’

For this ring, I thee sue

Speech is never totally free

Mahzarin Banaji opened the symposium on Tuesday by recounting the “implicit association” experiments she had done at Yale and at Harvard. The final talk is today at 9 a.m.
Kris Snibbe/Harvard Staff Photographer
Turning a light on our implicit biases
Brett Milano
Harvard Correspondent
Social psychologist details research at University-wide faculty seminar
Few people would readily admit that they’re biased when it comes to race, gender, age, class, or nationality. But virtually all of us have such biases, even if we aren’t consciously aware of them, according to Mahzarin Banaji, Cabot Professor of Social Ethics in the Department of Psychology, who studies implicit biases. The trick is figuring out what they are so that we can interfere with their influence on our behavior.
Banaji was the featured speaker at an online seminar Tuesday, “Blindspot: Hidden Biases of Good People,” which was also the title of Banaji’s 2013 book, written with Anthony Greenwald. The presentation was part of Harvard’s first-ever University-wide faculty seminar.
“Precipitated in part by the national reckoning over race, in the wake of George Floyd, Breonna Taylor and others, the phrase ‘implicit bias’ has almost become a household word,” said moderator Judith Singer, Harvard’s senior vice provost for faculty development and diversity. Owing to the high interest on campus, Banaji was slated to present her talk on three different occasions, with the final one at 9 a.m. Thursday.
Banaji opened on Tuesday by recounting the “implicit association” experiments she had done at Yale and at Harvard. The assumptions underlying the research on implicit bias derive from well-established theories of learning and memory and the empirical results are derived from tasks that have their roots in experimental psychology and neuroscience. Banaji’s first experiments found, not surprisingly, that New Englanders associated good things with the Red Sox and bad things with the Yankees.
She then went further by replacing the sports teams with gay and straight, thin and fat, and Black and white. The responses were sometimes surprising: Shown a group of white and Asian faces, a test group at Yale associated the former more with American symbols though all the images were of U.S. citizens. In a further study, the faces of American-born celebrities of Asian descent were associated as less American than those of white celebrities who were in fact European. “This shows how discrepant our implicit bias is from even factual information,” she said.
How can an institution that is almost 400 years old not reveal a history of biases, Banaji said, citing President Charles Eliot’s words on Dexter Gate: “Depart to serve better thy country and thy kind” and asking the audience to think about what he may have meant by the last two words.
She cited Harvard’s current admission strategy of seeking geographic and economic diversity as examples of clear progress — if, as she said, “we are truly interested in bringing the best to Harvard.” She added, “We take these actions consciously, not because they are easy but because they are in our interest and in the interest of society.”
Moving beyond racial issues, Banaji suggested that we sometimes see only what we believe we should see. To illustrate she showed a video clip of a basketball game and asked the audience to count the number of passes between players. Then the psychologist pointed out that something else had occurred in the video — a woman with an umbrella had walked through — but most watchers failed to register it. “You watch the video with a set of expectations, one of which is that a woman with an umbrella will not walk through a basketball game. When the data contradicts an expectation, the data doesn’t always win.”
Expectations, based on experience, may create associations such as “Valley Girl Uptalk” is the equivalent of “not too bright.” But when a quirky way of speaking spreads to a large number of young people from certain generations, it stops being a useful guide. And yet, Banaji said, she has been caught in her dismissal of a great idea presented in uptalk. Banaji stressed that the appropriate course of action is not to ask the person to change the way she speaks but rather for her and other decision makers to know that using language and accents to judge ideas is something people at their own peril.
Banaji closed the talk with a personal story that showed how subtler biases work: She’d once turned down an interview because she had issues with the magazine for which the journalist worked.
The writer accepted this and mentioned she’d been at Yale when Banaji taught there. The professor then surprised herself by agreeing to the interview based on this fragment of shared history that ought not to have influenced her. She urged her colleagues to think about positive actions, such as helping that perpetuate the status quo.
“You and I don’t discriminate the way our ancestors did,” she said. “We don’t go around hurting people who are not members of our own group. We do it in a very civilized way: We discriminate by who we help. The question we should be asking is, ‘Where is my help landing? Is it landing on the most deserved, or just on the one I shared a ZIP code with for four years?’”
To subscribe to short educational modules that help to combat implicit biases, visit outsmartinghumanminds.org .
Share this article
You might like.
Justice Ketanji Brown Jackson discusses new memoir, ‘unlikely path’ from South Florida to Harvard to nation’s highest court

Unhappy suitor wants $70,000 engagement gift back. Now court must decide whether 1950s legal standard has outlived relevance.

Cass Sunstein suggests universities look to First Amendment as they struggle to craft rules in wake of disruptive protests
Harvard releases race data for Class of 2028
Cohort is first to be impacted by Supreme Court’s admissions ruling
Parkinson’s may take a ‘gut-first’ path
Damage to upper GI lining linked to future risk of Parkinson’s disease, says new study
High doses of Adderall may increase psychosis risk
Among those who take prescription amphetamines, 81% of cases of psychosis or mania could have been eliminated if they were not on the high dose, findings suggest
How Effective is Unconscious Bias Training? A comprehensive evaluation of recent assessments
Reviewed by Nick Spragg
A Review of
Unconscious Bias Training: An assessment of the evidence for effectiveness
Doyin Atewologun Tinu Cornish Fatima Tresh
If applicable, enter a short description here..
Introduction
Unconscious bias training: An assessment of the evidence for effectiveness by Doyin Atewologun, et al. is a literature review and meta-analysis of studies that examines the evidence for the effectiveness of unconscious bias training programs in actually reducing unconscious bias in individuals and organizations. The authors first define unconscious bias as the automatic and unintentional stereotypes, attitudes, and beliefs that people hold about particular groups of people. They argue that these biases can have negative effects on people’s behaviors and decision-making, leading to discrimination and inequality. To address this issue, many organizations have started to implement unconscious bias training (UBT) programs, which aim to increase awareness of these biases and reduce their influence.
UBT interventions target the automatic behavioral functions in the brain which employ heuristics, or mental short-cuts, to process the large amounts of information individuals receive quickly so that people can carry out tasks efficiently. These mental short cuts can reinforce negative social stereotypes, especially for women, ethnic minorities, differently abled individuals, neurodiverse individuals, and others with protected characteristics. Atewologun et al. reference a previous intervention carried out by Baroness McGregor-Smith, member of the UK House of Lords, entitled, “Race in the Workplace.” In the 2017 study, Mcgregor-Smith examined the deep structural and historical biases that prevented individuals with protected characteristics from progressing in their careers. Mcgregor-Smith recommended that the UK Government implement a free digital unconscious bias training resource, which became a widely utilized resource in both the UK public and private sectors. The authors reevaluate these interventions a year following their initial implementation.
Doyin Atewologun is the Dean of the Rhodes Scholarship at the University of Oxford and is an expert on diversity, leadership, organizational culture, and intersectionality. Tinu Cornish is an Occupational Psychologist who focuses on psychological approaches to diversity and inclusion leadership. Fatima Tresh is a psychologist and expert in human cognition and behavior addressing diversity, equity, and inclusion barriers.
Methods and Findings
Atewologun et al.’s assessment aims to achieve three objectives evaluating UBT program implementations across the UK: (1), to demonstrate evidence in favor of UBT’s effectiveness (2) to analyze the contextual conditions under which UBT is most effective; and (3), to highlight evidence gaps for further research. The authors underscore that “effectiveness” in this assessment is contingent on the aims of the training designer. A 3-part rapid evidence assessment methodology was utilized to assess the UBT’s effectiveness:
Identify evidence from online databases
- Published peer reviewed articles (N=57)
- Non-academic searches like reports (N=31)
Evaluate the quality of the evidence
- Utilize the Maryland Scale of Scientific Methods (ranking scale of 1-5: 1 exhibiting the lowest rigor (before-after comparison) 5 exhibiting the highest rigor (randomized control trial))
- Exclude sources with low scientific rigor (Level 1)
Analyze the evidence
- Identify aims and design of the intervention, draw conclusions about outcomes, and review the gathered evidence (N=18)
Among the key findings in the article, the authors highlight four types of UBT interventions they will measure: (1) awareness raising, (2) implicit bias change, (3) explicit bias change, and (4) behavior change.
Awareness Raising
Among the selected studies, eleven studies explicitly aimed to raise awareness of implicit bias, and the authors conclude in their analyses that UBT interventions can substantially increase awareness of bias. Whatley’s 2018 Implicit Association Test highlighted a successful intervention. In the study, Whatley measured UBT’s effectiveness on a multidisciplinary team’s attitudes toward African American students in special education. Whatley’s pre- and post- evaluations of a bias literacy workshop indicated the UBT intervention substantially improved both staff vulnerability to bias and individual student expectations.
Implicit Bias Change
Of the eleven studies aiming to change implicit bias, Atewologun et al. found that there is mixed evidence for UBT’s effectiveness. Two studies suggested that UBT can reduce the strength of bias; yet, there was no evidence that UBT can reduce bias to the extent of “neutral” preference. In Girod et al.’s 2016 evaluation of an educational presentation on reducing gender bias, 281 faculty members across 13 clinical departments at Stanford University indicated in the pre-trial a slight preference for males in leadership positions (this was consistent across all racial groups), and this male preference reduced in the post-trial measure. Yet, the authors concluded that males and older participants held stronger racialized and gendered implicit biases in both the pre- and post- trial measures.
Explicit Bias Change
Nine studies reviewed in the assessment indicated that UBT is effective in changing explicit bias, but less effective than awareness raising or implicit bias changing . Of the available research, it was unclear to the authors how to best measure explicit bias. In Moss-Racusin et al. ‘s 2016 “scientific diversity” workshop administered to 126 life sciences instructors, the aim of the study was to increase awareness of gender diversity, reduce gender bias, and increase diversity-promoting actions. In this particular study, all three aims were effectively achieved.
Behavior Change
Of the ten studies aiming to change behavior, only two of these studies actually measured behavior change Because of this limitation, the authors concluded that there is insufficient evidence to indicate UBT’s effectiveness. Research examining behavior change is limited, and methods evaluating behavior change have low validity because they do not measure actual observed behavior change. In Forscher’s 2017 UBT intervention administered to 292 United States university students, researchers found that the effects of unconscious bias awareness waned two weeks post-intervention. However, a follow-up study conducted two years later between the intervention group and a control group indicated possible long-term behavior change. Participants in the intervention group were more likely to publicly refute an essay endorsing racial stereotyping than the control group.
Conclusions
In the concluding remarks, the authors highlight a variety of high-level observations about the assessed literature. Among these observations, the most notable include:
- Male participants hold stronger unconscious gender biases than female participants. This gap can be reduced with UBT, and UBT may be more effective for men with respect to gender biases. There is some evidence that online and face-to-face UBT are equally effective for awareness raising.
- Mandatory UBT is generally more effective for behavior change than voluntary UBT. This is not supported by more rigorous studies, however.
- Bias reduction strategies are more effective for reducing implicit bias and ineffective in reducing explicit bias.
- Some mindfulness interventions can reduce implicit bias and possibly mitigate discriminatory actions.
- Bias mitigation strategies may have back-firing effects if participants do not want to be influenced or do not agree with the proposed direction of influence.
In the final remarks, the authors set forth a series of recommendations for practice and future research. The first recommendation is to have a more nuanced approach to UBT content: use an implicit association test to increase awareness of unconscious bias and measure changes in implicit bias, educate participants about unconscious bias theory, and integrate bias reduction strategies in the UBT to increase participant confidence in managing their biases. The second recommendation focuses on the UBT context, such as delivering training to those who work closely together in a team unit or otherwise. Finally, the third recommendation is to evaluate effectiveness: randomly assign matched participants to control and intervention groups and deliver training to control groups when effectiveness has been established.
The authors suggest multiple areas for further research: systematic comparisons of approaches and design characteristics, investigations of UBT’s effectiveness in reducing bias against all protected groups, uniform measurement outcomes of UBT, structural changes due to UBT interventions, additional cognitive or social processes integral to maintaining inequity, and the impact of mandatory versus voluntary attendance on UBT effectiveness.
- Training & Evaluation
- Training Evaluations
- explicit bias
- implicit bias
- organizational behavior
- Unconscious bias
- unconscious bias training
Share this Article
- Spragg, Nick
- Atewologun, Doyin
- Tinu Cornish
- Fatima Tresh
Related Articles
Antiracist school leadership: making ‘race’ count in leadership preparation and development.
Introduction Schools around the world have started to grapple more acutely with racism due to the changing needs of an increasingly racially diverse and integrated student population, as well as in response to urgent calls for educational reform. These calls particularly urge educational reforms that include to developing and growing an antiracist curriculum and trainings.…
Best Practices or Best Guesses? Assessing the Efficacy of Corporate Affirmative Action and Diversity Policies
Introduction Over the past several decades, there has been an increase in efforts to diversify the American corporate workforce. In 2018, the employment search engine Indeed saw an 18% increase in diversity and inclusion job postings from the previous year, and a 2017 report indicated that about $8 billion is spent annually on diversity training.…
Thank you for visiting RRAPP
Please help us improve the site by answering three short questions.
- Why did you visit or use the site today? Select an answer To lead DEI or racial equity efforts at my organization To advise leaders on DEI best practices at my organization To learn new strategies for antiracist organizational change For public policy purposes For general research purposes For academic research purposes For student assignment Out of curiosity Other
- How did you use the site today? Select an answer Find research materials Cite a RRAPP summary Cite an original article Share an article with a colleague or organization Share an article on social media Suggest an article for RRAPP to review and post An article or summary from RRAPP was shared with me Other
- Are you? Select an answer CEO/ED Senior management Staff Consultant Graduate Student Undergraduate Student Scholar/Researcher Other
- What industry are you in? Select an answer Academia Private Public/Government Non-profit Other
- Email This field is for validation purposes and should be left unchanged.
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplement Archive
- Editorial Commentaries
- Perspectives
- Cover Archive
- IDSA Journals
- Clinical Infectious Diseases
- Open Forum Infectious Diseases
- Author Guidelines
- Open Access
- Why Publish
- IDSA Journals Calls for Papers
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- Journals Career Network
- About The Journal of Infectious Diseases
- About the Infectious Diseases Society of America
- About the HIV Medicine Association
- IDSA COI Policy
- Editorial Board
- Self-Archiving Policy
- For Reviewers
- For Press Offices
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Unconscious bias—the role it plays and how to measure it, impact of bias on healthcare delivery, measuring bias—the implicit association test (iat), mitigating unconscious bias, call to action.
- < Previous
The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It
- Article contents
- Figures & tables
- Supplementary Data
Jasmine R Marcelin, Dawd S Siraj, Robert Victor, Shaila Kotadia, Yvonne A Maldonado, The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It, The Journal of Infectious Diseases , Volume 220, Issue Supplement_2, 15 September 2019, Pages S62–S73, https://doi.org/10.1093/infdis/jiz214
- Permissions Icon Permissions
The increasing diversity in the US population is reflected in the patients who healthcare professionals treat. Unfortunately, this diversity is not always represented by the demographic characteristics of healthcare professionals themselves. Patients from underrepresented groups in the United States can experience the effects of unintentional cognitive (unconscious) biases that derive from cultural stereotypes in ways that perpetuate health inequities. Unconscious bias can also affect healthcare professionals in many ways, including patient-clinician interactions, hiring and promotion, and their own interprofessional interactions. The strategies described in this article can help us recognize and mitigate unconscious bias and can help create an equitable environment in healthcare, including the field of infectious diseases.
There is compelling evidence that increasing diversity in the healthcare workforce improves healthcare delivery, especially to underrepresented segments of the population [ 1 , 2 ]. Although we are familiar with the term “underrepresented minority” (URM), the Association of American Medical Colleges, has coined a similar term, which can be interchangeable: “Underrepresented in medicine means those racial and ethnic populations that are underrepresented in the medical profession relative to their numbers in the general population” [ 3 ]. However, this definition does not include other nonracial or ethnic groups that may be underrepresented in medicine, such as lesbian, gay, bisexual, transgender, or questioning/queer (LGBTQ) individuals or persons with disabilities. US census data estimate that the prevalence of African American and Hispanic individuals in the US population is 13% and 18%, respectively [ 4 ], while the prevalence of Americans identifying as LGBT was estimated by Gallup in 2017 to be about 4.5% [ 5 ]. Yet African American and Hispanic physicians account for a mere 6% and 5%, respectively, of medical school graduates, and account for 3% and 4%, respectively, of full-time medical school faculty [ 6 ]. As for LGBTQ medical graduates, the Association of American Medical Colleges does not report their prevalence [ 6 ]. Persons with disabilities are estimated to be 8.7% of the general population [ 4 ], while the prevalence of physicians with disabilities has been estimated to be a mere 2.7% [ 7 ]. Furthermore, although women currently outnumber men in first-year medical school classes [ 8 ], gender disparities still exist at higher ranks in women’s medical careers [ 9–11 ].
Unconscious or implicit bias describes associations or attitudes that reflexively alter our perceptions, thereby affecting behavior, interactions, and decision-making [ 12–14 ]. The Institute of Medicine (now the National Academy of Medicine) notes that bias, stereotyping, and prejudice may play an important role in persisting healthcare disparities and that addressing these issues should include recruiting more medical professionals from underrepresented communities [ 1 ]. Bias may unconsciously influence the way information about an individual is processed, leading to unintended disparities that have real consequences in medical school admissions, patient care, faculty hiring, promotion, and opportunities for growth ( Figure 1 ). Compared with heterosexual peers, LGBT populations experience disparities in physical and mental health outcomes [ 15 , 16 ]. Stigma and bias (both conscious and unconscious) projected by medical professionals toward the LGBTQ population play a major role in perpetuating these disparities [ 17 ]. Interventions on how to mitigate this bias that draw roots from race/ethnicity or gender bias literature can also be applied to bias toward gender/sexual minorities and other underrepresented groups in medicine.

Glossary of key terms.
The specialty of infectious diseases is not free from disparities. Of >11 000 members of the Infectious Diseases Society of America (IDSA), 41% identify as women, 4% identify as African American, 8% identify as Hispanic, and <1% identify as Native American or Pacific Islander (personal communication, Chris Busky, IDSA chief executive officer, 2019). However, IDSA data on members who identify as LGBTQ and members with disabilities are not available.
The 2017 IDSA annual compensation survey reports that women earn a lower income than men [ 18 ], and a review of the full report demonstrates similar disparities among URM physicians, compared with their white peers [ 19 ]. While it may not be feasible to assign a direct causal relationship between unconscious bias and disparities within the infectious diseases specialty, it is reasonable and ethical to attempt to address any potential relationship between the two. In this article, we define unconscious bias and describe its effect on healthcare professionals. We also provide strategies to identify and mitigate unconscious bias at an organizational and individual level, which can be applied in both academic and nonacademic settings.
Even in 2019, overt racism, misogyny, and transphobia/homophobia continue to influence current events. However, in the decades since the healthcare community has moved toward becoming more egalitarian, overt discrimination in medicine based on gender, race, ethnicity, or other factors have become less conspicuous. Nevertheless, unconscious bias still influences all human interactions [ 13 ]. The ability to rapidly categorize every person or thing we encounter is thought to be an evolutionary development to ensure survival; early ancestors needed to decide quickly whether a person, animal, or situation they encountered was likely to be friendly or dangerous [ 20 ]. Centuries later, these innate tendencies to categorize everything we encounter is a shortcut that our brains still use.
Stereotypes also inadvertently play a significant role in medical education ( Figure 1 ). Presentation of patients and clinical vignettes often begin with a patient’s age, presumed gender, and presumed racial identity. Automatic associations and mnemonics help medical students remember that, on examination, a black child with bone pain may have sickle-cell disease or a white child with recurrent respiratory infections may have cystic fibrosis. These learning associations may be based on true prevalence rates but may not apply to individual patients. Using stereotypes in this fashion may lead to premature closure and missed diagnoses, when clinicians fail to see their patients as more than their perceived demographic characteristics. In the beginning of the human immunodeficiency virus (HIV) epidemic, the high prevalence of HIV among gay men led to initial beliefs that the disease could not be transmitted beyond the gay community. This association hampered the recognition of the disease in women, children, heterosexual men, and blood donor recipients. Furthermore, the fact that white gay men were overrepresented in early reported prevalence data likely led to lack of recognition of the epidemic in communities of color, a fact that is crucial to the demographic characteristics of today’s epidemic. Today, there is still no clear solution to learning about the epidemiology of diseases without these imprecise associations, which can impact the rapidity of accurate diagnosis and therapy.
Unconscious bias describes associations or attitudes that unknowingly alter one’s perceptions and therefore often go unrecognized by the individual, whereas conscious bias is an explicit form of bias that is based on one’s discriminatory beliefs and values and can be targeted in nature [ 14 ]. While neither form of bias belongs in the healthcare profession, conscious bias actively goes against the very ethos of medical professionals to serve all human beings regardless of identity. Conscious bias has manifested itself in severe forms of abuse within the medical profession. One notable historical example being the Tuskegee syphilis study, in which black men were targeted to determine the effects of untreated, latent syphilis. The Tuskegee study demonstrated how conscious bias, in this case manifested in the form of racism, led to the unethical treatment of black men that continues to have long-lasting effects on health equity and justice in today’s society [ 21 ]. Given the intentional nature of conscious bias, a different set of tools and a greater length of time are likely required to change one’s attitudes and actions. Tackling unconscious bias involves willingness to alter one’s behaviors regardless of intent, when the impact of one’s biases are uncovered and addressed [ 22 ]
There is still debate, however, about the degree to which unconscious bias affects clinician decision-making. In one systematic review on the impact of unconscious bias on healthcare delivery, there was strong evidence demonstrating the prevalence of unconscious bias (encompassing race/ethnicity, gender, socioeconomic status, age, weight, persons living with HIV, disability, and persons who inject drugs) affecting clinical judgment and the behavior of physicians and nurses toward patients [ 12 ]. However, another systematic review found only moderate-quality evidence that unconscious racial bias affects clinical decision-making [ 23 ]. A detailed discussion of the impact of unconscious bias on healthcare delivery is out of the scope of this article, which is focused on the impact of unconscious bias as it relates to healthcare professionals themselves. Nevertheless, strategies to mitigate the effects of unconscious bias (discussed later) can be applied to healthcare delivery and patient interactions.
While we know that unconscious bias is ubiquitous, it can be difficult to know how much it affects a person’s daily interactions. In many cases, an individual’s unconscious beliefs may differ from their explicit actions. For example, healthcare professionals, if asked, might say they try to treat all patients equally and may not believe they hold negative attitudes about patients. However, by definition, they may lack awareness of their own potential unconscious biases, and their actions may unknowingly suggest that these biases are active.
To measure unconscious bias, Drs Mahzarin Banaji and Anthony Greenwald developed the IAT in 1998 [ 24 ]. Many versions of the IAT are accessible online (available at: https://implicit.harvard.edu/implicit/ ), but one of the most studied is the Race IAT. The IAT has been extensively studied as an inexpensive tool that provides feedback on an individual biases for self-reflection. The IAT calculates how quickly people associate different terms with each other. To determine unconscious race bias, the race IAT asks the subject to sort pictures (of white and black people) and words (good or bad) into pairs. For example, in one part of the Race IAT, participants must associate good words with white people and bad words with black people. In another part of the Race IAT, they must associate good words with black people and bad words with white people. Based on the reaction times needed to perform these tasks, the software calculates a bias score [ 20 , 24 ]. Category pairs that are unconsciously preferred are easier to sort (and therefore take less time) than those that are not [ 24 ]. These unconscious associations can be identified even in individuals who outwardly express egalitarian beliefs [ 20 , 24 ]. According to Project Implicit, the Race IAT has been taken >4 million times between 2002 and 2017, and 75% of test takers demonstrate an automatic white preference, meaning that most people (including a small group of black people) automatically associate white people with goodness and black people with badness [ 20 ]. Proponents of the IAT state that automatic preference for one group over another can signal potential discriminatory behavior even when the individuals with the automatic preference outwardly express egalitarian beliefs [ 20 ]. These preferences do not necessarily mean that an individual is prejudiced, which is associated with outward expressions of negative attitudes toward different social groups [ 20 ].
Many of the studies of unconscious bias described in this article use the IAT as the primary tool for measuring the phenomenon. Nevertheless, the degree to which the IAT predicts behavior is as of yet unclear, and it is important to recognize the limitations and criticisms of the IAT, as this is pertinent to its potential application in mitigating unconscious bias. Blanton et al reanalyzed data from 2 studies supporting the validity of the IAT, claiming that there is no evidence predicting individual behavior, with concerns for interjudge reliability and inclusion of outliers affecting results [ 25 ]. Response to this criticism by McConnell et al describes extensive training of test judges and evidence that the reanalysis was not a perfect replication of methods [ 26 ]. Blanton et al argue further in a different article that attempting to explain behavior on the basis of results of the IAT is problematic because the test relies on an arbitrary metric, leading to identified preferences when individuals are “behaviorally neutral” [ 27 ]. Notwithstanding the limitations of the IAT, none of its critics refute the existence of unconscious bias and that it can influence life experiences. The following sections review how unconscious bias affects different groups in the healthcare workforce.
Racial Bias
Medical school admissions committees serve as an important gatekeeper to address the significant disparities between racial and ethnic minorities in healthcare as compared to the general population. Yet one study demonstrated that members of a medical school admissions committee displayed significant unconscious white preference (especially among men and faculty members) despite acknowledging almost zero explicit white preference [ 28 ]. An earlier study of unconscious racial and social bias in medical students found unconscious white and upper-class preference on the IAT but no obvious unconscious preferences in students’ response to vignette-based patient assessments [ 29 ]. Unconscious bias affects the lived experiences of trainees, can potentially influence decisions to pursue certain specialties, and may lead to isolation. A recent study by Osseo-Asare et al described African American residents’ experiences of being only “one of a few” minority physicians; some major themes included discrimination, the presence of daily microaggressions, and the burden of being tasked as race/ethnic “ambassadors,” expected to speak on behalf of their demographic group [ 30 ].
Gender Bias
Gender bias in medical education and leadership development has been well documented [ 11 , 31 ]. Medical student evaluations vary depending on the gender of the student and even the evaluator [ 31 ]. Similar studies have demonstrated gender bias in qualitative evaluations of residents and letters of recommendations, with a more positive tone and use of agentic descriptors in evaluations of male residents as compared to female residents [ 11 ]. Studies evaluating inclusion of women as speakers have also demonstrated gender bias, with fewer women invited to speak at grand rounds [ 9 ] and differences in the formal introductions of female speakers as compared to male speakers [ 32 , 33 ], with men more likely referred to by their official titles than women.
Sexual and Gender Minority Bias
Sexual and gender minority groups are underrepresented in medicine and experience bias and microaggressions similar to those experience by racial and ethnic minorities. Experiences with or perceptions of bias lead to junior physicians not disclosing their sexual identity on the personal statement part of their residency applications for fear of application rejection or not disclosing that they are gay to colleagues and supervisors for fear of rejection or poor evaluations [ 34 ]. In one study, some physician survey respondents indicated some level of discomfort about people who are gay, transgender, or living with HIV being admitted to medical school. These respondents were less likely to refer patients to physician colleagues who were gay, transgender, or living with HIV [ 35 ]. These explicit biases were significantly reduced, compared with those revealed in prior surveys done in 1982 and 1999; opposition to gay medical school applicants went from 30% in 1982 to 0.4% in 2017, and discomfort with referring patients to gay physicians went from 46% in 1982 to 2% in 2017 [ 35 ]. The 2017 survey did not measure levels of unconscious bias, which is likely to still be pervasive despite decreased explicit bias. As with other types of bias, these data reveal that explicit bias against gay physicians has decreased over time; the degree of unconscious bias, however, likely persists. While this is encouraging to some degree, unconscious bias may be much more challenging to confront than explicit bias. Thus, members of underrepresented groups may be left wondering about the intentions of others and being labeled as “too sensitive.”
Studies including the perspectives of LGBTQ healthcare professionals demonstrate that major challenges to their academic careers persist to this day. These include lack of LGBTQ mentorship, poor recognition of scholarship opportunities, and noninclusive or even hostile institutional climates [ 36 ]. Phelan et al studied changes in biased attitudes toward sexual and gender minorities during medical school and found that reduced unconscious and explicit bias was associated with more-frequent and favorable interactions with LGBTQ students, faculty, residents, and patients [ 37 ].
Disability Bias
Physicians with disabilities constitute another minority group that may experience bias in medicine, and the degree to which they experience this may vary, depending on whether disabilities may be visible or invisible. One study estimated the prevalence of self-disclosed disability in US medical students to be 2.7% [ 7 ]. Medical schools are charged with complying with the Americans With Disabilities Act, but only a minority of schools support the full spectrum of accommodations for students with disabilities [ 38 ]. Many schools do not include a specific curriculum for disability awareness [ 39 ]. Physicians with disabilities have felt compelled to work twice as hard as their able-bodied peers for acceptance, struggled with stigma and microaggressions, and encountered institutional climates where they generally felt like they did not belong [ 40 ]. These are themes that are shared by individuals from racial and ethnic minorities.
A strategy to counter unconscious bias requires an intentional multidimensional approach and usually operates in tandem with strategies to increase diversity, inclusion, and equity [ 41 , 42 ]. This is becoming increasingly important in training programs in the various specialties, including infectious diseases. The Accreditation Council for Graduate Medical Education recently updated their common program requirements for fellowship programs and has stipulated that, effective July 2019, “[t]he program’s annual evaluation must include an assessment of the program’s efforts to recruit and retain a diverse workforce” [ 43 ]. The implication of this requirement is that recognition and mitigation of potential biases that may influence retention of a diverse workforce will ultimately be evaluated (directly or indirectly).
Mitigating unconscious bias and improving inclusivity is a long-term goal requiring constant attention and repetition and a combination of general strategies that can have a positive influence across all groups of people affected by bias [ 44 ]. These strategies can be implemented at organizational and individual levels and, in some cases, can overlap between the 2 domains ( Figure 2 ). In this section, we review how infectious diseases clinicians and organizations like IDSA and hospitals can use some of these strategies to address and mitigate implicit bias in our specialty.

Organization-level and personal-level strategies to mitigate unconscious bias. Orange circles indicate organization-specific strategies, green circles indicate individual-level strategies, and blue circles represent strategies that can be emphasized on both organizational and individual levels to mitigate implicit bias.
Organizational Strategies
Commitment to a culture of inclusion: more than just diversity training or cultural competency.
Creating change requires more than just a climate survey, a vision statement, or creation of a diversity committee [ 45 ]. Organizations must commit to a culture shift by building institutional capacity for change [ 41 , 46 ]. This involves reaffirming the need not only for the recruitment of a critical mass of underrepresented individuals, but equally importantly, the recruitment of critical actor leaders who take the role of change agents and have the power to create equitable environments [ 41 , 47–49 ]. These change agents need not themselves be underrepresented; indeed, the success of culture change requires the involvement of allies within the majority group (eg, men, white people, and cis-gender heterosexual individuals). IDSA has demonstrated a commitment to this type of culture change with recent changes in leadership structure and with intentional recruitment of individuals invested in diversity and inclusion; however, there is always room for reevaluation of other areas where diversity is desired.
Committing to a culture of inclusion at the academic-institution level involves creating a deliberate strategy for medical trainee admission and evaluation and faculty hiring, promotion, and retention. Capers et al describe strategies for achieving diversity through medical school admissions, many of which can also be applied to faculty hiring and promotion [ 49 ]. Notable strategies they suggest include having admissions (or hiring) committee members take the IAT and reflect on their own potential biases before they review applications or interview candidates [ 49 ]. They also recommend appointing women, minorities, and junior medical professionals (students or junior faculty) to admissions committees, emphasizing the importance of different perspectives and backgrounds [ 49 ]. Organizations can also survey employee perception of inclusivity. These assessments include questions on the degree to which an individual feels a sense of belonging within an institution, alongside questions pertaining to experiences of bias on the grounds of cultural or demographic factors [ 50 ]. Conducting regular assessments and analysis of survey results, particularly on how individuals of diverse backgrounds feel they can exist within the organization and their culture simultaneously, allows organizations to ensure that their trainings on unconscious bias and promotion of cultural humility lead to long-term positive change. Furthermore, realizing that different demographic groups may feel less respected than others provides information on areas of focus for consequent refresher seminars on combating unconscious bias in conjunction with cultural humility.
Meaningful Diversity Training and the Usefulness of the IAT
Notwithstanding potential criticisms of the IAT with respect to prediction of discriminatory behavior, this can be a useful tool within a comprehensive organizational training seminar directed toward understanding and addressing individual unconscious bias. In the study by Capers et al, over two thirds of admissions committee members who took the IAT and responded to the post-IAT survey felt positive about the potential value of this tool in reducing their unconscious bias [ 28 ]. Additionally, almost half were cognizant of their IAT results when interviewing for the next admissions cycle, and 21% maintained that knowledge of this bias affected their decisions in the next admissions cycle [ 28 ]. Perhaps this knowledge led to conscious changes in committee member behavior because, in the following year, the matriculating class was the most diverse in that institution’s history [ 28 , 49 ]. A similar bias education intervention coupled with the IAT led to a decreased unconscious gender leadership bias in one academic center [ 48 ]. IDSA and infectious diseases practices (or academic divisions) could consider ways to incorporate this into already established training for those in leadership roles or on leadership search committees.
Of course, the potential applicability of the IAT can be overstated—at best, several meta-analyses have demonstrated that there may only be a weak correlation between IAT scores and individual behavior [ 51–53 ], and several criticisms of the IAT have already been discussed here. Additionally, while important to acknowledge that bias is pervasive, care must be taken to avoid normalizing bias and stereotypes because this may have the unintended consequence of reinforcing them [ 54 ]. Important points that should be emphasized when using the IAT as part of diversity training include that (1) people should be aware of their own biases and reflect on their behaviors individually; (2) the IAT can suggest generally how groups of people with certain results may behave, rather than how each individual will behave; and (3) on its own, the IAT is not a sufficient tool to mitigate the effects of bias, because if there is to be any chance of success, an active cultural/behavioral change must be engaged in tandem with bias awareness and diversity training [ 55 ].
Individual Strategies
Deliberative reflection.
Before encounters that are likely to be affected by bias (such as trainee evaluations, letters of recommendation, feedback, interviews, committee decisions, and patient encounters), deliberative reflection can help an individual recognize their own potential for bias and correct for this [ 56 ]. It is also a good time to consider the perspective of the individual whom they will be evaluating or interacting with and the potential impact of their biases on that individual. Participants can be encouraged to evaluate how their own experiences and identities influence their interactions. Including data on lapses in proper care due to provider bias also proves helpful in giving workers real-life examples of the consequences of not being vigilant for bias [ 51 , 57 ]. This motivated self-regulation based on reflections of individual biases has been shown to reduce stereotype activation and application [ 44 , 58 ]. If one unintentionally behaves in a discriminatory manner, self-reflection and open discussion can help to repair relationships ( Figure 3 ).

Strategies to address personal bias before and after it occurs.
Question and Actively Counter Stereotypes
Individuals may question how they can actively counter stereotypes and bias in observed interactions. The active-bystander approach adapted from the Kirwan Institute [ 59 ] can provide insight into appropriate responses in these situations ( Figure 4 ).

Kirwan Institute approach to countering unconscious bias as an active bystander.
Strategies That Apply to Both Organizations and Individuals
Cultural competency and beyond: cultural humility.
Healthcare organizations seeking to develop providers who can work seamlessly with colleagues and more effectively treat patients from all cultural backgrounds have been conducting trainings in cultural competency [ 60 ]. The term “cultural competency” implies that one has achieved a static goal of championing inclusivity. This approach imparts a false sense of confidence in leaders and healthcare professionals and fails to recognize that our understanding of cultural barriers is continually growing and evolving [ 61 ]. Cultural humility has been proposed as an alternate approach, subsuming the teachings of cultural competency while steering participants toward a continuous path of discovery and respect during interactions with colleagues and patients of different cultural backgrounds [ 62 ]. Other synonymous terms include “cultural sensitivity” and “cultural curiosity.” Rather than checking a box for training, cultural humility focuses on the individual and teaches that developing one’s self-awareness is a critical step in achieving mindfulness for others [ 63 ]. Cultural humility emphasizes that individuals must acknowledge the experiential lens through which they view the world and that their view is not nearly as extensive, open, or dynamic as they might perceive [ 61 ]. By training leaders and healthcare professionals that they do not need to be and ultimately cannot be experts in all the intersecting cultures that they encounter, healthcare professionals can focus on a readiness to learn that can translate to greater confidence and willingness in caring for patients of varying backgrounds [ 61 ].
As cultural humility is important to recognizing and mitigating conscious and unconscious biases, patient simulations and diversity-related trainings should be augmented with discussions about cultural humility. By integrating cultural humility into healthcare training procedures, organizations can strive to eliminate the perceived unease healthcare professionals might experience when interacting with individuals from backgrounds or cultures unfamiliar to them. Cultural humility starts from a condition of empathy and proceeds through the asking of open questions in each interaction ( Figure 1 ). Instilling elements of cultural humility training within simulation-based learning provides participants with experience in treating a wide array of patients while providing low-risk, feedback-based learning opportunities [ 22 , 64 ].
Diversify Experiences to Provide Counterstereotypical Interactions
Exposing individuals to counterstereotypical experiences can have a positive impact on unconscious bias [ 10 , 44 , 55 ]. Therefore, intentional efforts to include faculty from underrepresented groups as preceptors, educators, and invited speakers can help reduce the unconscious associations of these responsibilities as unattainable. Capers et al suggest that including students, women, and African Americans and other racial and ethnic minorities on admissions committees may be part of a strategy to reduce unconscious bias in medical school admissions [ 49 ]. If institutions, organizations, and conference program committees are aware of their own metrics in this respect, following this information with deliberate choices to remedy inequities can have a profound impact on increasing diversity [ 65 ]. Furthermore, in medical training, while deliberate curricula involving disparities and care of underrepresented individuals are beneficial, educators must be aware of the impact of the hidden curriculum on their trainees. The term “hidden curriculum” refers to the aspects of medicine that are learned by trainees outside the traditional classroom/didactic instruction environment. It encompasses observed interactions, behaviors, and experiences often driven by unconscious and explicit bias and institutional climate [ 66–68 ]. Students can be taught to actively seek out the hidden curriculum in their training environment, reflect on the lessons, and use this reflection to inform their own behaviors [ 67 ]. Individuals can intentionally diversify their own circles, connecting with people from different backgrounds and experiences. This can include the occasionally awkward and uncomfortable introductions at professional meetings or at community events, making an effort to read books by diverse authors, or trying new foods with a colleague. These are small behavioral changes that, with time, can help to retrain our brain to classify people as “same” instead of “other.”
Mentorship and Sponsorship
Mentors can, at any stage in one’s career, provide advice and career assistance with collaborations, but sponsors are typically more senior individuals who can curate high-profile opportunities to support a junior person, often with potential personal or professional risk if that person does not meet expectations. URMs and women physicians tend not to have as much support with mentoring and sponsorship as the majority group, white men. Qualitative studies of URM physician perspectives typically reveal themes of isolation and lack of mentorship, regardless of the URM group being studied [ 30 , 36 , 69 ]. Possible reasons include lack of mentors from similar backgrounds or ineffective mentoring in discordant mentor-mentee relationships. Mentor-training workshops that intentionally include unconscious bias training can enhance the effectiveness of mentors working with diverse trainees and junior faculty and address this potential barrier to URM success [ 70 ]. Providing mentorship within an individual department, as well as support for participating in external mentorship and career development programs, can help create sponsorship opportunities that eventually influence career advancement [ 41 ]. Many professional societies such as IDSA provide mentorship opportunities, and these can be enhanced by encouraging more sponsorship of junior clinicians for opportunities such as podium lectures, moderating at conferences, writing editorials, or committee positions.
In the years since the IAT was first described, researchers have published countless data on the impact of unconscious bias. Fortunately, explicit and implicit attitudes toward many disenfranchised groups of people have regressed to a more neutral position over time [ 71 ], but this does not mean that unconscious bias has disappeared. Just as healthcare providers are required to stay up to date on medical techniques and procedures to best serve their patients, we propose that trainings involving the social aspects of medicine be treated similarly. Cultural humility is characterized by lifelong learning and is a key aspect of a successful provider-patient relationship. Thus, it is imperative that healthcare organizations and professional medical societies such as IDSA continually provide healthcare professionals with learning opportunities to enhance their interactions with individuals different from themselves. Effectively addressing unconscious bias and subsequent disparities in IDSA will need comprehensive, multifaceted, and evidence-based interventions ( Figure 5 ).

Unconscious bias highlights.
IDSA has demonstrated a commitment to diversifying its society leadership by commissioning the Gender Disparities Task Force and the Inclusion, Diversity, Access & Equity Task Force, reconfiguring existing committees, developing new committees (eg, the Leadership Development Committee), and creating new opportunities, such as the IDSA Leadership Institute. While these are important and impactful actions, we propose the following additional steps to address the role of unconscious bias in various settings. First, develop an IDSA-sponsored climate survey to assess perceptions of inclusion and belonging within the Society, and repeat this climate assessment after implementing bias reduction strategies. Second, provide IDSA-sponsored education/training on unconscious bias reduction strategies and cultural humility to academic infectious disease divisions and fellowship programs to support the recruitment and retention of a diverse infectious diseases physician workforce. Third, develop benchmarks for excellence in infectious diseases divisions and fellowship training programs to evaluate these bias reduction strategies. Fourth, provide education/training on unconscious bias–reduction strategies and cultural humility to leadership and membership within IDSA. Specifically, the board of directors, the Leadership Development Committee, the Awards Committee, and others involved in electing, nominating, or honoring members should consider including incorporating the IAT and bias-reduction education for their committee members. After implementing such strategies, IDSA should reevaluate metrics of awardees, committee chairs, and leadership to determine whether these strategies made an impact. Fifth, cultivate existing mentorship programs within IDSA, with the added focus of intentional mentoring and sponsorship of groups traditionally underrepresented in leadership. Sixth, commit to consistent review and revision of infectious diseases recruitment messaging, ensuring that materials and media counter harmful stereotypes and represent true diversity. Seventh, collect, review, and publish metrics of diversity in all facets of the membership, including IDWeek speaker demographic characteristics, IDSA journal editor/reviewers, guideline authorship, and committee membership, with intentional response strategies to change these demographic characteristics to a more diverse distribution. Eighth, be transparent about reporting of metrics, with clear accountability and flexibility to adjust initiatives based on results.
Although there are numerous data describing the impact of unconscious bias on healthcare delivery, clinician-patient interactions, and patient outcomes, discussion of these aspects is out of the scope of this article, which focuses on the impact of unconscious bias on healthcare professionals. Additionally, the majority of data on unconscious bias presented in this article relates to general academic training and career development, as data in the infectious diseases practice community is limited. This represents an area of need for evaluation within the specialty of infectious diseases, since a vast majority of members are in clinical practice and may experience bias in varying degrees. While it is important to support trainees who may experience unconscious bias, it is also critical to provide support for infectious diseases clinicians further along in their careers, as a means to maintain retention in the specialty. Finally, some individuals may prefer person-first language, while others may prefer identity-first language when referring to disabilities. We consistently used person-first language throughout this manuscript based on the recommendation by the Centers for Disease Control & Prevention ( https://www.cdc.gov/ncbddd/disabilityandhealth/pdf/disabilityposter_photos.pdf ).
Supplement sponsorship . This supplement is sponsored by the Infectious Diseases Society of America.
Acknowledgments . We thank Drs Molly Carnes, Ranna Parekh, and Arghavan Salles, as well as Lena Tenney, for critical review of this manuscript before publication; Mr Chris Busky, for providing written communications about the demographic characteristics of IDSA membership and leadership; and Catherine Hiller, for her assistance with manuscript preparation.
J. R. M. wrote first draft and subsequent revisions; D. S. and R. V. contributed to the first draft and subsequent revisions; S. K. contributed to the first draft and subsequent revisions; Y. A. M. contributed to subsequent revisions; and all authors reviewed a final version of the work before submission.
Potential conflicts of interest . J. R. M. and D. S. are members of the IDSA Inclusion, Diversity, Access & Equity Task Force. All other authors report no potential conflicts.
All authors have submitted the ICMJE form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Institute of Medicine (US) Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the U.S. Healthcare Workforce . In the nation’s compelling interest: ensuring diversity in the health-care workforce . Smedley BD , Stith Butler A , Bristow LR , eds. Washington, DC : National Academies Press (US) , 2004 .
Google Scholar
Google Preview
American College of Physicians . Racial and ethnic disparities in health care, updated 2010 . https://www.acponline.org/system/files/documents/advocacy/current_policy_papers/assets/racial_disparities.pdf . Accessed 25 January 2019 .
Association of American Medical Colleges . Underrepresented in medicine definition . https://www.aamc.org/initiatives/urm/ . Accessed 19 January 2019 .
United States Census Bureau . US Census Bureau QuickFacts . https://www.census.gov/quickfacts/fact/table/US# . Accessed 2 January 2019 .
Newport F. In U.S., estimate of LGBT population rises to 4.5% . https://news.gallup.com/poll/234863/estimate-lgbt-population-rises.aspx . Accessed 25 January 2019 .
Association of American Medical Colleges (AAMC) . AAMC facts & figures 2016; diversity in medical education . http://www.aamcdiversityfactsandfigures2016.org/index.html . Accessed 25 January 2019 .
Meeks LM , Herzer KR . Prevalence of self-disclosed disability among medical students in US allopathic medical schools . JAMA 2016 ; 316 : 2271 – 2 .
Association of American Medical Colleges . U.S. medical school applications and matriculants by school, state of legal residence, and sex, 2018–2019 . https://www.aamc.org/download/321442/data/factstablea1.pdf . Accessed 4 January 2019 .
Boiko JR , Anderson AJM , Gordon RA . Representation of women among academic grand rounds speakers . JAMA Intern Med 2017 ; 177 : 722 – 4 .
Carnes M , Bartels CM , Kaatz A , Kolehmainen C . Why is John more likely to become department chair than Jennifer? Trans Am Clin Climatol Assoc 2015 ; 126 : 197 – 214 .
Gerull KM , Loe M , Seiler K , McAllister J , Salles A . Assessing gender bias in qualitative evaluations of surgical residents . Am J Surg 2019 ; 217 : 306 – 13 .
FitzGerald C , Hurst S . Implicit bias in healthcare professionals: a systematic review . BMC Med Ethics 2017 ; 18 .
Staats C , Dandar V , St Cloud T , Wright R . How the prejudices we don’t know we have affect medical education, medical careers, and patient health . In: Darcy Lewis and Emily Paulsen, eds. Proceedings of the 2014 diversity and inclusion innovation forum: unconscious bias in academic medicine . Association of American Medical Colleges . Association of American Medical Colleges and the Kirwan Institute for the Study of Race and Ethnicity at The Ohio State University, USA 2017;1–93.
Staats C , Patton C. State of the science: implicit bias review: the Ohio State University Kirwan Instiute for the study of race and ethnicity . OH : The Kirwan Institute for the Study of Race and Ethnicity at The Ohio State University , 2013 ; 1 – 102 .
Institute of Medicine . The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding . Washington, DC : The National Academies Press , 2011 .
Gonzales G , Przedworski J , Henning-Smith C . Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the united states: results from the national health interview survey . JAMA Intern Med 2016 ; 176 : 1344 – 51 .
Valdiserri RO , Holtgrave DR , Poteat TC , Beyrer C . Unraveling health disparities among sexual and gender minorities: a commentary on the persistent impact of stigma . J Homosex 2019 ; 66 : 571 – 89 .
Trotman R , Kim AI , MacIntyre AT , Ritter JT , Malani AN . 2017 infectious diseases society of america physician compensation survey: results and analysis . Open Forum Infect Dis 2018 ; 5 : ofy309 .
Marcelin JR , Bares SH , Fadul N . Improved infectious diseases physician compensation but continued disparities for women and underrepresented minorities . Open Forum Infect Dis 2019 ; 6 : ofz042 .
Banaji MR , Greenwald AG. Blindspot: hidden biases of good people . 1st ed. USA : Delacorte Press , 2013 .
Francis CK . Medical ethos and social responsibility in clinical medicine . J Urban Health 2001 ; 78 : 29 – 45 .
Teal CR , Gill AC , Green AR , Crandall S . Helping medical learners recognise and manage unconscious bias toward certain patient groups . Med Educ 2012 ; 46 : 80 – 8 .
Dehon E , Weiss N , Jones J , Faulconer W , Hinton E , Sterling S . A systematic review of the impact of physician implicit racial bias on clinical decision making . Acad Emerg Med 2017 ; 24 : 895 – 904 .
Greenwald AG , McGhee DE , Schwartz JL . Measuring individual differences in implicit cognition: the implicit association test . J Pers Soc Psychol 1998 ; 74 : 1464 – 80 .
Blanton H , Jaccard J , Klick J , Mellers B , Mitchell G , Tetlock PE . Strong claims and weak evidence: reassessing the predictive validity of the IAT . J Appl Psychol 2009 ; 94 : 567 – 82 ; discussion 583–603.
McConnell AR , Leibold JM. Weak criticisms and selective evidence: Reply to Blanton et al . (2009) . J Appl Psychol , 2009;94, 583-9. doi:10.1037/a0014649
Blanton H , Jaccard J , Strauts E , Mitchell G , Tetlock PE . Toward a meaningful metric of implicit prejudice . J Appl Psychol 2015 ; 100 : 1468 – 81 .
Capers Q 4th , Clinchot D , McDougle L , Greenwald AG . Implicit racial bias in medical school admissions . Acad Med 2017 ; 92 : 365 – 9 .
Haider AH , Sexton J , Sriram N , et al. Association of unconscious race and social class bias with vignette-based clinical assessments by medical students . JAMA 2011 ; 306 : 942 – 51 .
Osseo-Asare A , Balasuriya L , Huot SJ , et al. Minority resident physicians’ views on the role of race/ethnicity in their training experiences in the workplace . JAMA Netw Open 2018 ; 1 : e182723 .
Riese A , Rappaport L , Alverson B , Park S , Rockney RM . Clinical performance evaluations of third-year medical students and association with student and evaluator gender . Acad Med 2017 ; 92 : 835 – 40 .
Files JA , Mayer AP , Ko MG , et al. Speaker introductions at internal medicine grand rounds: forms of address reveal gender bias . J Womens Health (Larchmt) 2017 ; 26 : 413 – 9 .
Mehta S , Rose L , Cook D , Herridge M , Owais S , Metaxa V . The speaker gender gap at critical care conferences . Crit Care Med 2018 ; 46 : 991 – 996 .
Lee KP , Kelz RR , Dubé B , Morris JB . Attitude and perceptions of the other underrepresented minority in surgery . J Surg Educ 2014 ; 71 : e47 – 52 .
Marlin R , Kadakia A , Ethridge B , Mathews WC . Physician attitudes toward homosexuality and HIV: the PATHH-III survey . LGBT Health 2018 ; 5 : 431 – 42 .
Sánchez NF , Rankin S , Callahan E , et al. LGBT trainee and health professional perspectives on academic careers–facilitators and challenges . LGBT Health 2015 ; 2 : 346 – 56 .
Phelan SM , Burke SE , Hardeman RR , et al. Medical school factors associated with changes in implicit and explicit bias against gay and lesbian people among 3492 graduating medical students . J Gen Intern Med 2017 ; 32 : 1193 – 201 .
Zazove P , Case B , Moreland C , et al. U.S. medical schools’ compliance with the americans with disabilities act: findings from a national study . Acad Med 2016 ; 91 : 979 – 86 .
Seidel E , Crowe S . The state of disability awareness in american medical schools . Am J Phys Med Rehabil 2017 ; 96 : 673 – 6 .
Meeks LM , Herzer K , Jain NR . Removing barriers and facilitating access: increasing the number of physicians with disabilities . Acad Med 2018 ; 93 : 540 – 3 .
DiBrito SR , Lopez CM , Jones C , Mathur A . Reducing implicit bias: association of women surgeons #HeForShe task force best practice recommendations . J Am Coll Surg 2019 ; 228 : 303 – 9 .
South-Paul JE , Roth L , Davis PK , et al. Building diversity in a complex academic health center . Acad Med 2013 ; 88 : 1259 – 64 .
Accreditation Council for Graduate Medical Education . Common program requirements (fellowship) . https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRFellowship2019.pdf . Accessed 19 January 2019 .
Devine PG , Forscher PS , Austin AJ , Cox WT . Long-term reduction in implicit race bias: a prejudice habit-breaking intervention . J Exp Soc Psychol 2012 ; 48 : 1267 – 78 .
Carnes M , Fine E , Sheridan J . Promises and pitfalls of diversity statements: proceed with caution . Acad Med 2019 ; 94 : 20 – 4 .
Smith DG . Building institutional capacity for diversity and inclusion in academic medicine . Acad Med 2012 ; 87 : 1511 – 5 .
Helitzer DL , Newbill SL , Cardinali G , Morahan PS , Chang S , Magrane D . Changing the culture of academic medicine: critical mass or critical actors? J Womens Health (Larchmt) 2017 ; 26 : 540 – 8 .
Girod S , Fassiotto M , Grewal D , et al. Reducing implicit gender leadership bias in academic medicine with an educational intervention . Acad Med 2016 ; 91 : 1143 – 50 .
Capers Q , McDougle L , Clinchot DM . Strategies for achieving diversity through medical school admissions . J Health Care Poor Underserved 2018 ; 29 : 9 – 18 .
Person SD , Jordan CG , Allison JJ , et al. Measuring diversity and inclusion in academic medicine: the diversity engagement survey . Acad Med 2015 ; 90 : 1675 – 83 .
Greenwald AG , Banaji MR , Nosek BA . Statistically small effects of the implicit association test can have societally large effects . J Pers Soc Psychol 2015 ; 108 : 553 – 61 .
Oswald FL , Mitchell G , Blanton H , Jaccard J , Tetlock PE . Predicting ethnic and racial discrimination: a meta-analysis of IAT criterion studies . J Pers Soc Psychol 2013 ; 105 : 171 – 92 .
Oswald FL , Mitchell G , Blanton H , Jaccard J , Tetlock PE . Using the IAT to predict ethnic and racial discrimination: small effect sizes of unknown societal significance . J Pers Soc Psychol 2015 ; 108 : 562 – 71 .
Duguid MM , Thomas-Hunt MC . Condoning stereotyping? How awareness of stereotyping prevalence impacts expression of stereotypes . J Appl Psychol 2015 ; 100 : 343 – 59 .
Dasgupta N . Chapter five—implicit attitudes and beliefs adapt to situations: a decade of research on the malleability of implicit prejudice, stereotypes, and the self-concept . In: Devine P , Plant A , eds. Advances in experimental social psychology . Vol. 47 . USA: Academic Press, 2013 : 233 – 79 .
Phillips NA , Tannan SC , Kalliainen LK . Understanding and overcoming implicit gender bias in plastic surgery . Plast Reconstr Surg 2016 ; 138 : 1111 – 6 .
Nelson SC , Prasad S , Hackman HW . Training providers on issues of race and racism improve health care equity . Pediatr Blood Cancer 2015 ; 62 : 915 – 7 .
Burns MD , Monteith MJ , Parker LR . Training away bias: the differential effects of counterstereotype training and self-regulation on stereotype activation and application . J Exp Soc Psychol 2017 ; 73 : 97 – 110 .
Tenney L. Being an active bystander: strategies for challenging the emergence of bias. Columbus, OH: Ohio State University Kirwan Institute for the Study of Race and Ethnicity , 2017 .
Harrison G , Turner R . Being a ‘culturally competent’ social worker: making sense of a murky concept in practice . Br J Soc Work 2010 ; 41 : 333 – 350 .
Juarez JA , Marvel K , Brezinski KL , Glazner C , Towbin MM , Lawton S . Bridging the gap: a curriculum to teach residents cultural humility . Fam Med 2006 ; 38 : 97 – 102 .
Chang ES , Simon M , Dong X . Integrating cultural humility into health care professional education and training . Adv Health Sci Educ Theory Pract 2012 ; 17 : 269 – 78 .
Kumagai AK , Lypson ML . Beyond cultural competence: critical consciousness, social justice, and multicultural education . Acad Med 2009 ; 84 : 782 – 7 .
Beauchamp GA , McGregor AJ , Choo EK , Safdar B , Rayl Greenberg M . Incorporating sex and gender into culturally competent simulation in medical education . J Womens Health (Larchmt) 2019 . doi:10.1089/jwh.2018.7271
van Ryn M , Hardeman R , Phelan SM , et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a medical student CHANGES study report . J Gen Intern Med 2015 ; 30 : 1748 – 56 .
Hafferty FW . Beyond curriculum reform: confronting medicine’s hidden curriculum . Acad Med 1998 ; 73 : 403 – 7 .
Neve H , Collett T . Empowering students with the hidden curriculum . Clin Teach 2018 ; 15 : 494 – 9 .
Fallin-Bennett K . Implicit bias against sexual minorities in medicine: cycles of professional influence and the role of the hidden curriculum . Acad Med 2015 ; 90 : 549 – 52 .
Liebschutz JM , Darko GO , Finley EP , Cawse JM , Bharel M , Orlander JD . In the minority: black physicians in residency and their experiences . J Natl Med Assoc 2006 ; 98 : 1441 – 8 .
Gandhi M , Fernandez A , Stoff DM , et al. Development and implementation of a workshop to enhance the effectiveness of mentors working with diverse mentees in HIV research . AIDS Res Hum Retroviruses 2014 ; 30 : 730 – 7 .
Charlesworth TES , Banaji MR . Patterns of implicit and explicit attitudes: I. Long-Term change and stability from 2007 to 2016 . Psychol Sci 2019 ; 30 : 174 – 92 .
Yeager KA , Bauer-Wu S . Cultural humility: essential foundation for clinical researchers . Appl Nurs Res 2013 ; 26 : 251 – 6 .
Sue DW , Capodilupo CM , Torino GC , et al. Racial microaggressions in everyday life: implications for clinical practice . Am Psychol 2007 ; 62 : 271 – 86 .
- bias (epidemiology)
- communicable diseases
- delivery of health care
- personnel selection
- cultural competence
- infectious diseases society of america
- mentorships
| Month: | Total Views: |
|---|---|
| August 2019 | 509 |
| September 2019 | 589 |
| October 2019 | 1,410 |
| November 2019 | 2,042 |
| December 2019 | 1,411 |
| January 2020 | 2,310 |
| February 2020 | 2,600 |
| March 2020 | 2,346 |
| April 2020 | 3,582 |
| May 2020 | 1,716 |
| June 2020 | 4,194 |
| July 2020 | 3,754 |
| August 2020 | 4,157 |
| September 2020 | 5,002 |
| October 2020 | 5,731 |
| November 2020 | 5,337 |
| December 2020 | 4,038 |
| January 2021 | 4,439 |
| February 2021 | 5,264 |
| March 2021 | 7,110 |
| April 2021 | 6,594 |
| May 2021 | 5,651 |
| June 2021 | 4,077 |
| July 2021 | 3,769 |
| August 2021 | 4,415 |
| September 2021 | 6,403 |
| October 2021 | 6,028 |
| November 2021 | 5,996 |
| December 2021 | 3,551 |
| January 2022 | 4,581 |
| February 2022 | 5,716 |
| March 2022 | 7,015 |
| April 2022 | 6,583 |
| May 2022 | 5,686 |
| June 2022 | 3,767 |
| July 2022 | 4,020 |
| August 2022 | 3,778 |
| September 2022 | 4,958 |
| October 2022 | 6,260 |
| November 2022 | 6,488 |
| December 2022 | 3,963 |
| January 2023 | 4,203 |
| February 2023 | 5,460 |
| March 2023 | 6,441 |
| April 2023 | 6,362 |
| May 2023 | 5,624 |
| June 2023 | 3,688 |
| July 2023 | 4,267 |
| August 2023 | 4,484 |
| September 2023 | 5,618 |
| October 2023 | 5,793 |
| November 2023 | 5,414 |
| December 2023 | 3,800 |
| January 2024 | 4,855 |
| February 2024 | 4,375 |
| March 2024 | 5,673 |
| April 2024 | 5,649 |
| May 2024 | 5,069 |
| June 2024 | 2,952 |
| July 2024 | 2,798 |
| August 2024 | 2,954 |
| September 2024 | 1,987 |
Email alerts
More on this topic, related articles in pubmed, citing articles via, looking for your next opportunity.
- Recommend to your Library
Affiliations
- Online ISSN 1537-6613
- Print ISSN 0022-1899
- Copyright © 2024 Infectious Diseases Society of America
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 08 March 2021
Understanding unconscious bias
- Barry Oulton 1
BDJ In Practice volume 34 , pages 26–27 ( 2021 ) Cite this article
23 Accesses
1 Altmetric
Metrics details
What if you could improve the way you communicate with your patients, peers and team by recognising your unconscious biases and challenging them? Dr Barry Oulton explores.
Most of us don't like to think of ourselves as discriminating against others or having biases towards or against certain groups, but unconscious bias or 'implicit bias', as it is also called, is innate to human nature.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Author information
Authors and affiliations.
The Confident Dentist, Vine Cottage, Hindhead, UK
Barry Oulton
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Barry Oulton .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Oulton, B. Understanding unconscious bias. BDJ In Pract 34 , 26–27 (2021). https://doi.org/10.1038/s41404-021-0685-8
Download citation
Published : 08 March 2021
Issue Date : March 2021
DOI : https://doi.org/10.1038/s41404-021-0685-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Understanding unconscious bias
This animation and briefing on unconscious bias adapted by Professor Uta Frith DBE FBA FMedSci FRS introduce the key concepts and current academic research around unconscious bias with the aim of alerting Royal Society selection and appointment panel members to potential biases that can arise when making judgments or decisions. They form part of the Society’s efforts to ensure that all those who serve on selection panels are aware of differences in how candidates may present themselves, how to recognise bias in oneself and others, how to recognise inappropriate advocacy or unreasoned judgement. All panellists receive an electronic copy of the briefing in advance of any meeting, it is also read at the beginning of each meeting as a reminder.
The Society is concerned with excellent science wherever and by whomever it is done and is committed to increasing diversity in STEM by seeking out participation from underrepresented groups, in order to build and develop a world in which studying and working in science are open to all. Addressing unconscious bias is one tool that the Royal Society is using to ensure that our funding, awards and appointments are drawn from the widest range of talent.
Further reading
Making better decisions in groups
Diversity in science
Implicit and unconscious, the bias in us all
- Unconscious bias briefing
Email updates
We promote excellence in science so that, together, we can benefit humanity and tackle the biggest challenges of our time.
Subscribe to our newsletters to be updated with the latest news on innovation, events, articles and reports.
What subscription are you interested in receiving? (Choose at least one subject)
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Unconscious bias among health professionals: a scoping review.

1. Introduction
2. materials and methods, 3.1. search results, 3.2. study characteristics, 3.3. results of the studies.
| Reference | Country | Type of Bias | Method | Description | N | HPs | Results | +/++/+++/0 |
|---|---|---|---|---|---|---|---|---|
| Afulani et al., 2021 [ ] | Kenya | SES bias | IAT and vignettes | Cross-sectional mixed-methods study with SES-IAT, vignettes varying by SES and follow-up qualitative interviews | 101 | Nurses, midwives, physicians, support staff | Moderate negative UB against women with low SES in IAT, differences in expectations towards patients according to stereotypes for both low- and high-SES women in vignettes | ++/n.a. |
| Al Alwan et al., 2019 [ ] | Saudi Arabia | SES bias | Vignettes | Cross-sectional vignette study varying by SES (low/high/neutral) | 45 | Physicians | No difference in accuracy or time for diagnosis between low, high, or neutral SES | 0 |
| Anastas et al., 2020 [ ] | USA | Racial bias, SES bias | IAT and vignettes | Cross-sectional study with race IAT (black/white) and re-analysis of computer-simulated vignette study varying by race (black/white) and SES (high/low) | 436 | Physicians | Weak negative UB for black people and strong negative UB for low SES in IATs. Effects between race and SES IAT scores and pain judgement. Different treatment decisions for race and SES in vignettes | +/+++/n.a. |
| Aweidah et al., 2016 [ ] | Australia | Weight bias | IAT | Cross-sectional mixed-methods pilot-study with weight IAT and qualitative interviews | 37 | Diagnostic radiographers | Negative weight bias | n.a. |
| Barnato et al., 2011 [ ] | USA | Racial bias | Vignettes | Cross-sectional study with randomized trial with standard ized patients varying by race (black/white) | 33 | Physicians | No difference in treatment decisions | 0 |
| Bartley et al., 2015 [ ] | USA | Ageism, gender bias, racial bias | Vignettes | Cross-sectional online vignette study with videos of virtual humans varying by age, gender, and race | 154 | Dentists, physicians | Differences in ratings of pain and pain treatment by age, sex and race of patient and by provider age, sex and race | n.a. |
| Bernardes & Lima 2011 [ ] | Portugal | Gender bias | Vignettes | Cross-sectional vignette study varying by gender | 126 | Nurses | Differences in attribution of pain according to gender in the absence of diagnosis | n.a. |
| Blair et al., 2013, 2013 and 2014 [ , , ] | USA | Racial bias | IAT | Cross-sectional mixed-methods study with race IATs (black/white and Hispanic/white), patients’ perception of treatment and electronic medical records | 210 | Health care providers | Strong negative UB against black and Hispanic people. The stronger the physicians’ UB, the lower the rating of the black patient of treatment (not for Hispanic). No difference in treatment according to medical records | +++/+++/0 |
| Bøker Lund et al., 2018 [ ] | Denmark | Weight bias | IAT and vignettes | Cross-sectional study with IAT on attitude and stereotypes for obesity and vignettes varying by gender and weight | 240 | Physicians | Strong negative UB against over weight people in IAT on attitudes and stereo-types. No differences in treatment options by weight, but in recommen dations by sex and weight in vignettes | +++/0/n.a. |
| Bous et al., 2021 [ ] | USA | Disability bias | IAT | Cross-sectional online study with disability IAT (cleft lips/normal lips) | 52 | Dentists | Moderate negative UB against people with disability (cleft lips) | ++ |
| Breathett et al., 2019 [ ] | USA | Racial bias | Vignettes | Cross-sectional mixed-methods study with vignette varied by race (black/white) and think-aloud interviews | 422/44 | Health care providers | No differences in recommendations for treatment in vignettes according to race | 0 |
| Brener et al., 2013 [ ] | Australia | Mental illness bias | IAT | Cross-sectional study with IAT on mental illness | 74 | Mental health providers | Weak negative UB bias against people with mental illness | + |
| Burgess et al., 2014 [ ] | USA | Racial bias | Vignettes | Cross-sectional web-based randomized vignette study varying by race (black/white) and cognitive load | 99 | Physicians | Differences in drug prescription according to physicians’ gender, cognitive load, and patient race | n.a. |
| Cassell 2015 [ ] | USA | Racial bias | Vignettes and IAT | Cross-sectional online-study with race IAT (black/white) and vignettes varying by race | 216 | Physicians | Moderate negative UB on IAT against black people. Difference in diagnosis but no difference in treat ment recommendation in vignettes | ++/n.a./0 |
| Centola et al., 2021 [ ] | USA | Racial bias, gender bias | Vignettes | Cross-sectional online-study with video-based vignettes manipulated by gender and race (black/white) | 120 | Physicians | Negative UB against black women with unsafe treatment recommen dations compared to white male patient | n.a. |
| Chapman et al., 2018 [ ] | USA | Racial bias | AMP | Sequential cohort online study with race AMP (Hispanic/ white) with pre- and post-intervention measure | 69 | Physicians | Negative racial bias against Hispanic people | n.a. |
| Claréus & Renström 2019 [ ] | Sweden | Gender bias | Vignettes | Cross-sectional online study with vignette varying by gender | 90 | Physicians | Negative UB on women in diagnosis related to back pain | n.a. |
| Colón-Emeric et al., 2017 [ ] | USA | Racial bias, gender bias | Vignettes | Repeated-measures study (pre- and post-intervention) with randomized vignettes differing by race, gender, and age | 541 | Nurses, rehabilitation staff | Small degree of negative UB against black people, no UB on gender | + |
| Cooper et al., 2012 [ ] | USA | Racial bias | IAT | Cross-sectional study with race IAT (black/white) on attitudes and racial stereotyping on compliance | 40 | Physicians | Moderate negative UB on race attitude and race compliance stereotyping | ++/++ |
| Crapanzano et al., 2018 [ ] | USA | Mental illness bias | IAT | Cross-sectional online-study with 4 IATs on attitude (good/bad), permanence, controllability, and ethology of mental illness (depression/ physical illness) | 86 | Physicians, psychiatrists | Weak–moderate negative UB on attitude, permanence, and controllability against mentally ill people amongst physicians not in psychiatrists. Moderate negative UB on ethology for both | +-++/+-++/+-++/0/++ |
| Daugherty et al., 2017 [ ] | USA | Gender bias | IAT and vignettes | Cross-sectional study with 2 gender IATs on stereotypes (strength and risk taking) and vignettes diffing by gender | 503 | Physicians | Moderate negative UB on gender stereotype in risk-taking and strong UB on strength IAT against women. No difference for diagnosis but differences in recommendations for testing in vignettes by gender | ++/+++/n.a. |
| Drwecki et al., 2011 [ ] | USA | Racial bias | Vignettes | Randomized experimental intervention study with vignettes varying by race (black/white) | 40 | Nurses | Differences in pain treatment recommendations by race | n.a. |
| Dy et al., 2015 [ ] | USA | Racial bias, gender bias | Vignettes | Cross-sectional computerized vignette study varied by race (black/white) and gender | 113 | Physicians | No difference in recommendations for surgery in vignettes for race and gender | 0 |
| Enea-Drapeau et al., 2012 [ ] | France | Disability bias | IAT | Cross-sectional study with 2 disability IAT (Trisomy 21, typical or weakly typical) | 55 | Health care providers | Implicit negative bias against people with Trisomy 21 | n.a. |
| Fiscella et al., 2021 [ ] | USA | Racial bias | IAT and vignettes | Randomized field experiment with standardised patient (black/white) and race IAT (black/white) | 90 | Physicians | Negative UB on race against black people in IAT. Physicians with stronger UB prescribed less frequently opioids to black patients and those with lower UB less frequently to white patients | n.a. |
| Galli et al., 2015 [ ] | Italy | Disability bias | IAT | Cross-sectional study with disability IAT (wheelchair users/no wheelchair users) | 45 | Physio-therapists, other health care providers | No UB against wheelchair users | 0 |
| Gould et al., 2019 [ ] | USA | Disability bias | IAT | Cross-sectional study with disability IAT | 290 | Genetic counsellors | Strong negative UB against people with disability | +++ |
| Graetz et al., 2021 [ ] | USA | Racial bias, SES bias | IAT and vignettes | Prospective study with IAT on race (black/white) and SES (high/low) and case vignettes | 105 | Health care providers | Strong negative UB against low-SES patients and a moderate negative bias on race (black people). No bias in vignettes | +++/++/0 |
| Guedj et al., 2021 [ ] | USA | Racial bias, weight bias | IAT | Cross-sectional online-study with weight IAT and 2 race IATs (black/white and Hispanic/white) | 101 | Physicians | Strong negative UB against black, Hispanic people and overweight people | +++/+++/+++ |
| Guillermo & Barre-Hemingway 2020 [ ] | USA | Racial bias | Vignettes | Cross-sectional study with randomized vignettes varying by race (black/white) | 116 | Health care providers | No race-based differences in pain estimates nor treatment recommendations | n.a. |
| Hagiwara et al., 2013, 2016, 2017 [ , , ] | USA | Racial bias | IAT | Re-analysis of cross-sectional study with race IAT and of racially discordant medical interactions | 14 | Physicians | Weak negative UB against black people. UB has influence in communi cation style of physicians and inter action when patients reported prior discrimination | + |
| Haider et al., 2014 [ ] | USA | Racial bias, SES bias | IAT and vignettes | Cross-sectional online study with race and SES IATs and vignettes varying by race (black/white) and SES (low/high) | 251 | Physicians | Moderate negative UB against black and strong negative UB against low SES people in IATs. No differences in treatment decisions in vignettes | ++/+++/0 |
| Haider et al., 2015 [ ] | USA | Racial bias, SES bias | IAT and vignettes | Cross-sectional online study with race and SES IATs and vignettes varying by race (black/white) and SES (low/high) | 215 | Physicians | Moderate negative UB against black people, strong UB against people with low SES in IATs. Differences on treatment decisions by race in 3 out of 27 decisions in vignettes | ++/+++/n.a. |
| Haider et al., 2015 [ ] | USA | Racial bias, SES bias | IAT and vignettes | Cross-sectional online study with race and SES IATs and vignettes varying by race (back/white) and SES (high/low) | 245 | Nurses | Moderate negative UB against black people and a strong negative UB against people with low SES in IATs. Differences in treatment decisions in vignettes according to race and SES | ++/+++/n.a. |
| Halvorson et al., 2019 [ ] | USA | Weight bias | IAT | Cross-sectional mixed-methods study with weight IAT and semi-structured key informant interviews | 28 | Physicians, nurses | Moderate to strong negative UB against overweight people | ++-+++ |
| Hausmann et al., 2015 [ ] | USA | Racial bias | IAT | Cross-sectional online pilot study with race IAT (black/white) | 14 | Physicians | Moderate negative UB against black people | ++ |
| Hirsh et al., 2015 [ ] | USA | Racial bias | IAT and vignettes | Cross-sectional study with race IAT and virtual human vignettes varying by race (black/white) and ambiguity of pain | 129 | Physicians | Moderate negative UB against black people in IAT. No difference in treat-ment options in vignettes with low ambiguity, with high ambiguity decisions varied for white patients not for black | ++/n.a. |
| Hirsh et al., 2020 [ ] | USA | Racial bias | IAT and vignettes | Cross-sectional online-study with race IAT and virtual vignettes varying by race (black/white) and addiction history | 135 | Physicians | Moderate negative UB against black people in IAT. Differences in perceptions about patients’ risks for misuse/abuse by race and past opioid misuse in vignettes | ++/n.a. |
| Hirsh et al., 2014 [ ] | USA | Gender bias | Vignettes | Cross-sectional study with computer simulated patient vignettes varying by gender | 98 | Health care providers | Differences in treatment recommendations by gender | n.a. |
| Hull et al., 2021 [ ] | USA | Racial bias | Vignettes | Cross-sectional online-study with vignette varying by race (black/white) | 174 | Health care providers | Negative UB against black people in consultation and prescribing behaviour depending on perceived ability of adherence | n.a. |
| Johnson et al., 2016 [ ] and 2017 [ ] | USA | Racial bias | IAT | Cross-sectional study with repeated measures (pre- and post- shift) with 2 race IATs (black/ white) (adult and child versions) | 91 | Physicians | Moderate negative UB against black people both for adults and children pre- and post-shift | ++ |
| Kopera et al., 2015 [ ] | Poland | Mental illness bias | GNAT | Cross-sectional study with GNAT on mental illness | 29 | Psychiatrists, psycho-therapists | Negative UB toward people with mental illness | n.a. |
| Lepièce et al., 2014 [ ] | Belgium | Racial bias | Vignettes | Cross-sectional vignette study varying by race (migrant status/ local) | 171 | Physicians | No differences in medical decisions by ethnicity except prescription of drugs | 0/n.a. |
| Liang et al., 2019 [ ] | USA | Diagnosis bias | IAT | Cross-sectional study with 2 IATs on prejudice and stereotypes on cervical cancer vs. ovarian cancer patients | 176 | Physicians, nurses | Weak negative unconscious prejudice and stereotyping toward cervical cancer patients. Physicians had no UB while nurses did | +/+/0/0 |
| Londono Tobon et al., 2021 [ ] | USA | Racial bias | IAT | Cross-sectional online study with 3 race IATs (black/white) related to diagnosis, compliance, and medication | 171 | Psychiatrists | Weak to moderate negative UB against black people on IATs on dia gnosis, compliance, and medication | +-++/+-++/+-++ |
| Lowe et al., 2020 [ ] | USA | Racial bias | (IAT) vignettes | Re-analysis of cross-sectional study with 2 race IATs (black/white and Hispanic/white) of videotaped counselling sessions with simulated patients | 60 | Genetic counsellors | Results of IATs see Schaa et al., 2015 Slight difference in communication strategies according to race in vignettes no association between communication style and IATs | n.a. |
| Moskowitz et al., 2012 [ ] | USA | Racial bias | Reaction time task with priming | Cross-sectional study with computerized reaction time task with subliminal exposure to black/white photographs | 11 | Physicians | Unconscious association of certain diseases to black people compared to white people | n.a. |
| Nash et al., 2014 [ ] | UK | Ageism | IAT | Cross-sectional study with ageism IAT | 49 | Nurses | Strong negative UB towards elderly people | +++ |
| Nymo et al., 2018 [ ] | Norway | SES bias | Vignettes | Cross-sectional online-study with vignettes varying by SES (low/neutral). | 107 | Physicians | Difference in priority of referrals by SES in one of 3 vignettes giving low-SES patients low priority | n.a. |
| Oliver et al., 2014 [ ] | USA | Racial bias | IAT and vignettes | Cross-sectional online study with randomized vignettes varying by race (black/white). Race and cooperativeness IATs | 543 | Physicians | Moderate negative UB against black people, weak negative UB on their cooperativeness in IATs. No difference in treatment decisions in vignettes according to race | ++/+/0 |
| Omori et al., 2012 [ ] | Japan | Mental illness bias | IAT | Repeated-measure sstudy before and after contact with mentally ill patients with 2 IATs with different expressions for mental illness and association to “criminal” | 51 | Physicians | Negative UB against people with mental illness (schizophrenia) | n.a. |
| Patel et al., 2019 [ ] | Italy | Racial bias | IAT and vignettes | Cross-sectional study with brief race IAT and randomized vignettes varying by race (black/white) | 57 | Dentists | Strong negative UB against black people in IAT. Differences in recommendations for treatment options by race in vignettes | +++/n.a. |
| Penner et al., 2016 [ ] | USA | Racial bias | IAT | Mixed-methods study with race IAT, recorded physician–patient interactions and follow-up interviews | 18 | Physicians | Weak negative UB against black people | + |
| Puumala et al., 2016 [ ] | USA | Racial bias | IAT and vignettes | Cross-sectional online study with vignettes. Two race IATs (American Native/white), child and adult versions | 101 | Physicians, nurses | Moderate negative UB against American Native people on IAT on child and adult versions. Only little differences in treatment recommen-dations in vignettes | ++/++/n.a. |
| Robstad et al., 2018 [ ] | Norway | Weight bias | IAT and vignettes | Cross-sectional online pilot study with 2 weight IATs on attitudes and stereotypes and vignettes varying by weight | 30 | Nurses | Strong negative UB on attitude and moderate on stereotypes against overweight people, no difference in behavioural intention in vignettes | +++/++/0 |
| Robstad et al., 2019 [ ] | Norway | Weight bias | IAT and vignettes | Cross-sectional study with two weight IATs on attitudes and stereotypes and vignettes varying by weight | 159 | Nurses | Strong negative UB against overweight people in both IAT, no difference in behavioural intention in vignettes | +++/+++/0 |
| Rojas et al., 2017 [ ] | USA | Racial bias | Vignettes | Cross-sectional online study with vignettes varying by race (black/white) | 342 | Physicians | No statistically significant differences in suspicion for abuse-related injury based on race of child | 0 |
| Sabin & Greenwald 2012 [ ] | USA | Racial bias | IAT and vignettes | Cross-sectional online study with 3 race IATs on attitude, compliance, and stereotypes and vignettes of child patients varying by race (black/white) | 86 | Physicians | Weak negative UB on attitude, moderate on compliance and stereo type against black people on IATs. Differences in treatment recommen dations by race in 1 out of 4 vignettes | +/++/++/n.a. |
| Sabin et al., 2012 [ ] | USA/Global | Weight bias | IAT | Re-analysis of data from weight IAT from Project Implicit (2006–2010) | 2284 | Physicians | Strong negative UB against overweight people | +++ |
| Sabin et al., 2015 [ ] | USA | Weight bias, racial bias | IAT | Cross-sectional online pilot study with weight and race IATs on (Native American/white) | 75 | Physicians, nurses, physician assistants | Strong negative UB against overweight people, weak negative UB against Native Americans | +++/+ |
| Sabin et al., 2015 [ ] | USA | LGBTQ bias | IAT | Re-analysis of data from LGB IAT from Project Implicit (2006–2012) | 18,983 | Physicians, nurses, mental health providers, other health care providers | Weak to moderate negative UB against homosexual people | +-++ |
| Sandhu et al., 2019 [ ] | Canada | Mental illness bias | IAT | Cross-sectional online study with IAT on mental illness | 538 | Psychiatrists | No UB against people with mental illness | 0 |
| Schaa et al., 2015 [ ] | USA | Racial bias | IAT | Mixed-methods study with cross-sectional online survey with IAT on race (black/white) and with re-analysis of data on patient–physician interaction | 60 | Genetic counsellors | Moderate negative UB against black people. Differences in communi cation style during counselling sessions according to race | ++/n.a. |
| Schoenberg et al., 2019 [ ] | USA | Racial bias, gender bias | Vignettes | Cross-sectional online pilot study with vignettes varying by race (skin tone) and gender | 80 | Physicians | Treatment options differed by skin colour and gender according to stereotypes | n.a. |
| Schroyen et al., 2016 [ ] | Belgium | Ageism | Vignettes | Cross-sectional study with ran domized vignettes varying by age | 76 | Nurses | Negative UB by age that increases as age of patient increases | n.a. |
| Setchell et al., 2014 [ ] | Australia | Weight bias | Vignettes | Cross-sectional online survey with vignettes differing in body mass index | 265 | Physio-therapists | Minimal statistically not significant differences in treatment options by weight of patients | 0 |
| Shapiro et al., 2018 [ ] | USA | Racial bias, SES bias | IAT and vignettes | Cross-sectional study with race and SES IATs and vignettes varying by race (black/white) and SES. | 971/549/530 | Physicians | Moderate negative UB against black women, strong negative UB against women with low SES in IATs. No differences of treatment recommen dations by race but by SES in vignettes | ++/+++/0/ n.a. |
| Siegelman et al., 2016 [ ] | USA | Racial bias | IAT and vignettes | Cross-sectional study with race IAT and vignettes varying by race (black/white) | 57 | Physicians | No results for IAT published and some difference in pain treatment by race in vignettes | n.a |
| Stepanikova 2012 [ ] | USA | Racial bias | Vignettes | Cross-sectional online vignette study with/without racial priming varying by race (black/Hispanic/ white) and cognitive load. | 81 | Physicians | UB in diagnosis and referral against black people and less so towards Hispanic people under time pressure, less so if there is no time pressure | n.a. |
| Sukhera et al., 2018 [ ] and 2019 [ ] | Canada | Mental illness bias | IAT | Cross-sectional mixed-methods study with IAT on dangerous ness of mental illness and semi-structured interviews about results | 31 | Psychiatrists, Nurses | 32% had a negative UB on dangerousness of mentally ill people and 55% on physically ill people, and 13% had no UB | n.a. |
| Tajeu et al., 2018 [ ] | USA | Racial bias | IAT | Cross-sectional online-study with race IAT (black/white) | 107 | Physicians, nurses, other health care providers | Moderate negative UB against black people | ++ |
| Tucker Edmonds et al., 2017 [ ] | USA | Racial bias | Vignettes | Cross-sectional pilot study with self-administered vignettes varying by race (black/white) | 77 | Physicians, nurses | Differences in treatment options by race | n.a. |
| Vaimberg et al., 2021 [ ] | USA | Disability bias | IAT and vignettes | Repeated measure online pilot study (pre- and post-intervention) with disability IAT (pre-intervention) and vignettes (with/without physical disability) pre- and post-intervention | 335 | Physicians, nurses, genetic counsellors, other health care providers | Negative UB on disabled people (84% of respon-dents), UB influencing clinical recommen dations. After intervention UB decreased, recommendations changed | n.a. |
| VanPuymbrouck et al., 2020 [ ] | Global | Disability bias | IAT | Re-analysis of data from disability IAT from Project Implicit (2004–2017) | 25,006 | Physicians, dentists, nurses, occupational- and physio-therapists, other health care providers | Moderate negative UB against disabled people | ++ |
| Walden et al., 2020 [ ] | USA | Disability bias | IAT | Cross-sectional study with disability IAT (stuttering/normal speech) | 15 | Speech–language pathologists | Moderate negative UB against people that stutter | ++ |
| Wandner et al., 2014 [ ] | USA | Racial bias, gender bias, ageism | Vignettes | Cross-sectional online vignette study with human virtual profiles varying by race, gender, and age | 193 | Physicians, nurses | Differences in pain assessment by race and gender, not by age. Male and black people were rated to have more pain | n.a./0 |
| Welch et al., 2012 [ ] | USA | Gender bias | Vignettes | Cross-sectional mixed-methods study with video vignette varying by gender with/without cognitive priming, think-aloud interviews | 256 | Physicians | Differences in treatment options by gender | n.a. |
| Welch et al., 2015 [ ] | USA | Mental illness bias | Vignettes | Cross-sectional video-based vignette study varying by symptoms of mental and physical illness | 256 | Physicians | Negative stereotypes against people with mental illness | n.a. |
| Wijayatunga et al., 2021 [ ] | USA | Weight bias | IAT | Randomized online study with repeated measures (pre-/post-intervention, 1-month follow-up) with weight IAT taken 3 times | 147 | Dieticians | Negative UB against overweight people at all 3 measurement points | n.a. |
| Wittlin et al., 2019 [ ] | USA | LGBTQ bias | IAT | Longitudinal study with 3 repeated measures with IAT on lesbian and gay people | 1155 | Physicians | Weak negative UB against lesbian and gay people at both time points | +/1 |
| Zestcott et al., 2021 [ ] | USA | Racial bias | IAT | Cross-sectional online-study with 2 IAT on race (American Native/ white) on prejudice and stereotypes | 111 | Physicians | Moderate negative UB toward American Natives in attitudes and stereotypes | ++/++ |
3.4. Biases
3.5. geographical distribution, 3.6. involved health professions, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest.
| Component/Database | PubMed/MEDLINE | CINAHL | PsycINFO and PsycARTICLES | AMED |
|---|---|---|---|---|
| Population | “Health personnel”[MESH] OR “Health personnel” OR “Health professional*” OR “Health personnel” OR Nurs* OR Physiotherap* OR “Physical therap*” OR “Occupational Therap*” OR Midwif* OR “Midwifery” [MESH] OR Logoped* OR “Speech therap*” OR Dietician* OR Paramedic* OR “Medical orderl*” OR Doctor* OR Osteopath* | (MH “Health Personnel+”) OR “Health professional*” OR “Health personnel” OR Nurs* OR Physiotherap* OR “Physical Therap*” OR “Occupational therap*” OR Midwife* OR Logoped* OR “Speech Therap*” OR Dietician* OR Paramedic* OR “Medical orderly*” OR Physician* OR Doctor* OR Osteopath* | exp clinicians/or exp health personnel/or exp therapists/OR Health personnel OR Health Professional* OR Nurs* OR Physiotherap* OR Occupational therap* OR Midwife* OR Logoped* OR Speech therap* OR Dietician* OR Paramedic* OR Medical orderly* OR Physician* OR Doctor* OR Osteopath* | exp health personnel OR Health Professional*.mp OR Nurs*.mp OR Physiotherap*.mp OR Physical therap*.mp” OR Occupational therap*.mp OR Midwife*.mp OR Logoped*.mp OR Speech therap*.mp OR Dietician*.mp OR Paramedic*.mp OR Medical orderly*.mp OR Physician*.mp OR Doctor*-mp OR Osteopath*.mp (mp=abstract, heading words, title) |
| AND | AND | AND | AND | |
| Concept (Phenomenon of Interest): Unconscious Bias/Implicit Bias | “Prejudice”[Mesh] OR “Stereotyping”[Mesh] OR “Social Discrimination”[Mesh] OR “unconscious Bias” OR “Implicit Bias” OR “Bias, implicit” OR “automatic bias” OR stereotyp* OR Prejudice* | (MM “Race Relations”) OR (MM “Attitude to AIDS”) OR (MM “Race Relations”) (MM “Prejudice+”) OR (MM “Attitude to ageing”) OR (MM “Attitude to disability”) OR (MM “Attitude to sexuality”) OR (MM “Attitude to obesity”) OR (MM “Cultural bias”) OR (MM “Cultural sensitivity”) OR (MM “Gender bias”) OR (MM “Attitude to mental illness”) (MM “Unconscious (Psychology))” OR (MM “Stereotyping”) OR (MM “Discrimination+”) OR “Implicit bias” OR “Unconscious bias” | exp *Implicit attitudes or exp *Prejudice or exp *Racial and ethnic attitudes or exp *Racial bias OR exp *Aged (attitudes toward) *Obesity (attitudes toward) OR exp *Disabled (attitudes toward) or exp *Health personnel attitudes or exp *physical illness (attitudes toward) or exp *Sexual attitudes OR “Unconscious bias” | exp Attitude of health personnel OR Exp Attitude to disability OR Exp Prejudice OR Implicit bias.mp OR Gender bias.mp OR Weight bias.mp OR Obesity bias.mp OR Ageism.mp OR Racial bias.mp OR Racial attitude.mp OR Health status disparities.mp (mp=abstract, heading words, title) |
| AND | AND | AND | AND | |
| Context: Health Care Delivery | “Delivery of Health Care”[Mesh] OR “Health Services”[Mesh] OR “Delivery of healthcare” OR “health care service*” | (MH “Health Care Delivery+”) OR (MH “Patient Care+”) OR (MH “Quality of Health Care+”) OR (MH “Professional-Patient Relations+”) OR “delivery of health care” | exp Treatment or “Delivery of health care” or “delivery of healthcare”.mp. [mp=ti, ab, hw, tc, id, ot, tm, mf, tx, ct] | exp “Delivery of health care”/or exp Health services/or exp Patient care/OR Health Care delivery.mp |
| Filter | 1 January 2011–31 December 2021 | 1 January 2011–31 December 2021 without Medline records and peer-reviewed | 1 January 2011–31 December 2021 peer-reviewed | 1 January 2011–31 December 2021 |
- Maina, I.W.; Belton, T.D.; Ginzberg, S.; Singh, A.; Johnson, T.J. A Decade of Studying Implicit Racial/Ethnic Bias in Healthcare Providers Using the Implicit Association Test. Soc. Sci. Med. 2018 , 199 , 219–229. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- James, S.A. The Strangest of All Encounters: Racial and Ethnic Discrimination in US Health Care. Cad. Saúde Pública 2017 , 33 (Suppl. S1), e00104416. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ho, I.K.; Lawrence, J.S. The Role of Social Cognition in Medical Decision Making with Asian American Patients. J. Racial Ethn. Health Disparities 2021 , 8 , 1112–1118. [ Google Scholar ] [ CrossRef ]
- Artiga, S.; Orgera, K.; Pham, O. Disparities in Health and Health Care: Five Key Questions and Answers. Kais. Fam. Found. Policy Brief. 2020 . Available online: https://files.kff.org/attachment/Issue-Brief-Disparities-in-Health-and-Health-Care-Five-Key-Questions-and-Answers (accessed on 8 May 2023).
- Institute of Medicine (US) Committee on Institutional and Policy-Level Strategies for Increasing the Diversity of the US Health Care Workforce, Board on Health Sciences Policy. In The Nation’s Compelling Interest: Ensuring Diversity in the Health-Care Workforce ; Smedley, B.D.; Butler, A.S.; Bristow, L.R. (Eds.) National Academies Press (US): Washington, DC, USA, 2004. [ Google Scholar ]
- Nelson, A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. J. Natl. Med. Assoc. 2002 , 94 , 666. [ Google Scholar ]
- Green, A.R.; Carney, D.R.; Pallin, D.J.; Ngo, L.H.; Raymond, K.L.; Iezzoni, L.I.; Banaji, M.R. Implicit Bias among Physicians and Its Prediction of Thrombolysis Decisions for Black and White Patients. J. Gen. Intern. Med. 2007 , 22 , 1231–1238. [ Google Scholar ] [ CrossRef ]
- Marcelin, J.R.; Siraj, D.S.; Victor, R.; Kotadia, S.; Maldonado, Y.A. The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It. J. Infect. Dis. 2019 , 220 , S62–S73. [ Google Scholar ] [ CrossRef ]
- Groves, P.S.; Bunch, J.L.; Sabin, J.A. Nurse Bias and Nursing Care Disparities Related to Patient Characteristics: A Scoping Review of the Quantitative and Qualitative Evidence. J. Clin. Nurs. 2021 , 30 , 3385–3397. [ Google Scholar ] [ CrossRef ]
- FitzGerald, C.; Hurst, S. Implicit Bias in Healthcare Professionals: A Systematic Review. BMC Med. Ethics 2017 , 18 , 19. [ Google Scholar ] [ CrossRef ]
- Banaji, M.R.; Greenwald, A.G. Blindspot: Hidden Biases of Good People ; Bantam: New York, NY, USA, 2016. [ Google Scholar ]
- Macrae, C.N.; Milne, A.B.; Bodenhausen, G.V. Stereotypes as Energy-Saving Devices: A Peek inside the Cognitive Toolbox. J. Pers. Soc. Psychol. 1994 , 66 , 37–47. [ Google Scholar ] [ CrossRef ]
- Galli, G.; Lenggenhager, B.; Scivoletto, G.; Molinari, M.; Pazzaglia, M. Don’t Look at My Wheelchair! The Plasticity of Longlasting Prejudice. Med. Educ. 2015 , 49 , 1239–1247. [ Google Scholar ] [ CrossRef ]
- Fiske, S.T. Stereotyping, Prejudice, and Discrimination. In The Handbook of Social Psychology , 4th ed.; McGraw-Hill: New York, NY, USA, 1998; Volume 1–2, pp. 357–411. ISBN 978-0-19-521376-8. [ Google Scholar ]
- APA Dictionary of Psychology. Available online: https://dictionary.apa.org/ (accessed on 8 May 2023).
- Hall, W.J.; Chapman, M.V.; Lee, K.M.; Merino, Y.M.; Thomas, T.W.; Payne, B.K.; Eng, E.; Day, S.H.; Coyne-Beasley, T. Implicit Racial/Ethnic Bias Among Health Care Professionals and Its Influence on Health Care Outcomes: A Systematic Review. Am. J. Public Health 2015 , 105 , e60–e76. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sukhera, J.; Wodzinski, M.; Milne, A.; Teunissen, P.W.; Lingard, L.; Watling, C. Implicit Bias and the Feedback Paradox: Exploring How Health Professionals Engage With Feedback While Questioning Its Credibility. Acad. Med. 2019 , 94 , 1204–1210. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Greenwald, A.G.; McGhee, D.E.; Schwartz, J.L.K. Measuring Individual Differences in Implicit Cognition: The Implicit Association Test. J. Pers. Soc. Psychol. 1998 , 74 , 1464. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nosek, B.A.; Banaji, M.R. The Go/No-Go Association Task. Soc. Cogn. 2001 , 19 , 625–666. [ Google Scholar ] [ CrossRef ]
- Burgess, D.J.; Phelan, S.; Workman, M.; Hagel, E.; Nelson, D.B.; Fu, S.S.; Widome, R.; van Ryn, M. The Effect of Cognitive Load and Patient Race on Physicians’ Decisions to Prescribe Opioids for Chronic Low Back Pain: A Randomized Trial. Pain Med. 2014 , 15 , 965–974. [ Google Scholar ] [ CrossRef ]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med. Res. Methodol. 2018 , 18 , 143. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated Methodological Guidance for the Conduct of Scoping Reviews. JBI Evid. Implement. 2021 , 19 , 3–10. [ Google Scholar ] [ CrossRef ]
- Meidert, U.; Dönnges, G.; Bucher, T. Unconscous Bias in Health Professionals a Systematic Review. OSF Cent. Open Sci. 2022 . Available online: https://osf.io/gjr9z/?view_only=a34d0ee2685b447eaad94b107928355f (accessed on 8 May 2023).
- Gawronski, B.; Hahn, A. Implicit Measures: Procedures, Use, and Interpretation. In Measurement in Social Psychology ; Routledge: London, UK, 2018; pp. 29–55. [ Google Scholar ]
- Gawronski, B.; De Houwer, J. Implicit Measures in Social and Personality Psychology. In Handbook of Research Methods in Social and Personality Psychology ; Reis, H.T., Judd, C.M., Eds.; Cambridge University Press: New York, NY, USA, 2013; pp. 283–310. ISBN 978-0-511-99648-1. [ Google Scholar ]
- Gould, D. Using Vignettes to Collect Data for Nursing Research Studies: How Valid Are the Findings? J. Clin. Nurs. 1996 , 5 , 207–212. [ Google Scholar ] [ CrossRef ]
- Evans, S.C.; Roberts, M.C.; Keeley, J.W.; Blossom, J.B.; Amaro, C.M.; Garcia, A.M.; Stough, C.O.; Canter, K.S.; Robles, R.; Reed, G.M. Vignette Methodologies for Studying Clinicians’ Decision-Making: Validity, Utility, and Application in ICD-11 Field Studies. Int. J. Clin. Health Psychol. 2015 , 15 , 160–170. [ Google Scholar ] [ CrossRef ]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016 , 75 , 40–46. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Corporation for Digital Scholarship Zotero. Available online: https://www.zotero.org/ (accessed on 8 May 2023).
- Veritas Health Innovation. Covidence Systematic Review Software. Available online: www.covidence.org (accessed on 8 May 2023).
- Cassell, N. Medical Treatment Decisions: Impact of Source of Motivation to Control Prejudice ; University of Maryland, Baltimore County: Baltimore, MD, USA, 2015. [ Google Scholar ]
- Kopera, M.; Suszek, H.; Bonar, E.; Myszka, M.; Gmaj, B.; Ilgen, M.; Wojnar, M. Evaluating Explicit and Implicit Stigma of Mental Illness in Mental Health Professionals and Medical Students. Community Ment. Health J. 2015 , 51 , 628–634. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chapman, M.V.; Hall, W.J.; Lee, K.; Colby, R.; Coyne-Beasley, T.; Day, S.; Eng, E.; Lightfoot, A.F.; Merino, Y.; Simán, F.M.; et al. Making a Difference in Medical Trainees’ Attitudes toward Latino Patients: A Pilot Study of an Intervention to Modify Implicit and Explicit Attitudes. Soc. Sci. Med. 2018 , 199 , 202–208. [ Google Scholar ] [ CrossRef ]
- Payne, B.K.; Cheng, C.M.; Govorun, O.; Stewart, B.D. An Inkblot for Attitudes: Affect Misattribution as Implicit Measurement. J. Personal. Soc. Psychol. 2005 , 89 , 277. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moskowitz, G.B.; Stone, J.; Childs, A. Implicit Stereotyping and Medical Decisions: Unconscious Stereotype Activation in Practitioners’ Thoughts about African Americans. Am. J. Public Health 2012 , 102 , 996–1001. [ Google Scholar ] [ CrossRef ]
- Shapiro, N.; Wachtel, E.V.; Bailey, S.M.; Espiritu, M.M. Implicit Physician Biases in Periviability Counseling. J. Pediatr. 2018 , 197 , 109–115. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Blair, I.V.; Steiner, J.F.; Hanratty, R.; Price, D.W.; Fairclough, D.L.; Daugherty, S.L.; Bronsert, M.; Magid, D.J.; Havranek, E.P. An Investigation of Associations between Clinicians’ Ethnic or Racial Bias and Hypertension Treatment, Medication Adherence and Blood Pressure Control. J. Gen. Intern. Med. 2014 , 29 , 987–995. [ Google Scholar ] [ CrossRef ]
- Drwecki, B.B.; Moore, C.F.; Ward, S.E.; Prkachin, K.M. Reducing Racial Disparities in Pain Treatment: The Role of Empathy and Perspective-Taking. Pain 2011 , 152 , 1001–1006. [ Google Scholar ] [ CrossRef ]
- Cooper, L.A.; Roter, D.L.; Carson, K.A.; Beach, M.C.; Sabin, J.A.; Greenwald, A.G.; Inui, T.S. The Associations of Clinicians’ Implicit Attitudes about Race with Medical Visit Communication and Patient Ratings of Interpersonal Care. Am. J. Public. Health 2012 , 102 , 979–987. [ Google Scholar ] [ CrossRef ]
- Vaimberg, E.; Demers, L.; Ford, E.; Sabatello, M.; Stevens, B.; Dasgupta, S. Project Inclusive Genetics: Exploring the Impact of Patient-Centered Counseling Training on Physical Disability Bias in the Prenatal Setting. PLoS ONE 2021 , 16 , e0255722. [ Google Scholar ] [ CrossRef ]
- Centola, D.; Guilbeault, D.; Sarkar, U.; Khoong, E.; Zhang, J. The Reduction of Race and Gender Bias in Clinical Treatment Recommendations Using Clinician Peer Networks in an Experimental Setting. Nat. Commun. 2021 , 12 , 6585. [ Google Scholar ] [ CrossRef ]
- Omori, A.; Tateno, A.; Ideno, T.; Takahashi, H.; Kawashima, Y.; Takemura, K.; Okubo, Y. Influence of Contact with Schizophrenia on Implicit Attitudes towards Schizophrenia Patients Held by Clinical Residents. BMC Psychiatry 2012 , 12 , 205. [ Google Scholar ] [ CrossRef ]
- Wijayatunga, N.N.; Bailey, D.; Klobodu, S.S.; Dawson, J.A.; Knight, K.; Dhurandhar, E.J. A Short, Attribution Theory-Based Video Intervention Does Not Reduce Weight Bias in a Nationally Representative Sample of Registered Dietitians: A Randomized Trial. Int. J. Obes. 2021 , 45 , 787–794. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Afulani, P.A.; Ogolla, B.A.; Oboke, E.N.; Ongeri, L.; Weiss, S.J.; Lyndon, A.; Mendes, W.B. Understanding Disparities in Person-Centred Maternity Care: The Potential Role of Provider Implicit and Explicit Bias. Health Policy Plan. 2021 , 36 , 298–311. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Al Alwan, I.; Magzoub, M.E.; Al Haqwi, A.; Badri, M.; Al Yousif, S.M.; Babiker, A.; Mamede, S.; Schmidt, H.G. Do Poor Patients Suffer from Inaccurate Diagnoses More than Well-to-Do Patients? A Randomized Control Trial. BMC Med. Educ. 2019 , 19 , 386. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Anastas, T.M.; Miller, M.M.; Hollingshead, N.A.; Stewart, J.C.; Rand, K.L.; Hirsh, A.T. The Unique and Interactive Effects of Patient Race, Patient Socioeconomic Status, and Provider Attitudes on Chronic Pain Care Decisions. Ann. Behav. Med. 2020 , 54 , 771–782. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Aweidah, L.; Robinson, J.; Cumming, S.; Lewis, S. Australian Diagnostic Radiographers’ Attitudes and Perceptions of Imaging Obese Patients: A Study of Self, Peers and Students. Radiography 2016 , 22 , e258–e263. [ Google Scholar ] [ CrossRef ]
- Barnato, A.E.; Mohan, D.; Downs, J.; Bryce, C.L.; Angus, D.C.; Arnold, R.M. A Randomized Trial of the Effect of Patient Race on Physicians’ Intensive Care Unit and Life-Sustaining Treatment Decisions for an Acutely Unstable Elder with End-Stage Cancer. Crit. Care Med. 2011 , 39 , 1663–1669. [ Google Scholar ] [ CrossRef ]
- Bartley, E.J.; Boissoneault, J.; Vargovich, A.M.; Wandner, L.D.; Hirsh, A.T.; Lok, B.C.; Heft, M.W.; Robinson, M.E. The Influence of Health Care Professional Characteristics on Pain Management Decisions. Pain Med. 2015 , 16 , 99–111. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bernardes, S.F.; Lima, M.L. A Contextual Approach on Sex-Related Biases in Pain Judgements: The Moderator Effects of Evidence of Pathology and Patients’ Distress Cues on Nurses’ Judgements of Chronic Low-Back Pain. Psychol. Health 2011 , 26 , 1642–1658. [ Google Scholar ] [ CrossRef ]
- Blair, I.V.; Havranek, E.P.; Price, D.W.; Hanratty, R.; Fairclough, D.L.; Farley, T.; Hirsh, H.K.; Steiner, J.F. Assessment of Biases against Latinos and African Americans among Primary Care Providers and Community Members. Am. J. Public Health 2013 , 103 , 92–98. [ Google Scholar ] [ CrossRef ]
- Blair, I.V.; Steiner, J.F.; Fairclough, D.L.; Hanratty, R.; Price, D.W.; Hirsh, H.K.; Wright, L.A.; Bronsert, M.; Karimkhani, E.; Magid, D.J.; et al. Clinicians’ Implicit Ethnic/Racial Bias and Perceptions of Care among Black and Latino Patients. Ann. Fam Med. 2013 , 11 , 43–52. [ Google Scholar ] [ CrossRef ]
- Bøker Lund, T.; Brodersen, J.; Sandøe, P. A Study of Anti-Fat Bias among Danish General Practitioners and Whether This Bias and General Practitioners’ Lifestyle Can Affect Treatment of Tension Headache in Patients with Obesity. Obes. Facts 2018 , 11 , 501–513. [ Google Scholar ] [ CrossRef ]
- Bous, R.M.; Lyamichev, A.; Kmentt, A.; Valiathan, M. Bias in a Blink: Shedding Light on Implicit Attitudes toward Patients with a Cleft Lip. Am. J. Orthod. Dentofac. Orthop. 2021 , 160 , 200–208. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Breathett, K.; Yee, E.; Pool, N.; Hebdon, M.; Crist, J.D.; Knapp, S.; Larsen, A.; Solola, S.; Luy, L.; Herrera-Theut, K.; et al. Does Race Influence Decision Making for Advanced Heart Failure Therapies? J. Am. Heart Assoc. 2019 , 8 , e013592. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Brener, L.; Wilson, H.; Rose, G.; Mackenzie, A.; de Wit, J. Challenging Stereotypes and Changing Attitudes: Improving Quality of Care for People with Hepatitis C through Positive Speakers Programs. Psychol. Health Med. 2013 , 18 , 242–249. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Claréus, B.; Renström, E.A. Physicians’ Gender Bias in the Diagnostic Assessment of Medically Unexplained Symptoms and Its Effect on Patient-Physician Relations. Scand. J. Psychol. 2019 , 60 , 338–347. [ Google Scholar ] [ CrossRef ]
- Colón-Emeric, C.S.; Corazzini, K.; McConnell, E.; Pan, W.; Toles, M.; Hall, R.; Batchelor-Murphy, M.; Yap, T.L.; Anderson, A.L.; Burd, A.; et al. Study of Individualization and Bias in Nursing Home Fall Prevention Practices. J. Am. Geriatr. Soc. 2017 , 65 , 815–821. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Crapanzano, K.; Fisher, D.; Hammarlund, R.; Hsieh, E.P.; May, W. An Exploration of Residents’ Implicit Biases Towards Depression—A Pilot Study. J. Gen. Intern. Med. 2018 , 33 , 2065–2069. [ Google Scholar ] [ CrossRef ]
- Daugherty, S.L.; Blair, I.V.; Havranek, E.P.; Furniss, A.; Dickinson, L.M.; Karimkhani, E.; Main, D.S.; Masoudi, F.A. Implicit Gender Bias and the Use of Cardiovascular Tests Among Cardiologists. J. Am. Heart Assoc. 2017 , 6 , e006872. [ Google Scholar ] [ CrossRef ]
- Dy, C.J.; Lyman, S.; Boutin-Foster, C.; Felix, K.; Kang, Y.; Parks, M.L. Do Patient Race and Sex Change Surgeon Recommendations for TKA? Clin. Orthop. Relat. Res. 2015 , 473 , 410–417. [ Google Scholar ] [ CrossRef ]
- Enea-Drapeau, C.; Carlier, M.; Huguet, P. Tracking Subtle Stereotypes of Children with Trisomy 21: From Facial-Feature-Based to Implicit Stereotyping. PLoS ONE 2012 , 7 , e34369. [ Google Scholar ] [ CrossRef ]
- Fiscella, K.; Epstein, R.M.; Griggs, J.J.; Marshall, M.M.; Shields, C.G. Is Physician Implicit Bias Associated with Differences in Care by Patient Race for Metastatic Cancer-Related Pain? PLoS ONE 2021 , 16 , e0257794. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Gould, H.; Hashmi, S.S.; Wagner, V.F.; Stoll, K.; Ostermaier, K.; Czerwinski, J. Examining Genetic Counselors’ Implicit Attitudes toward Disability. J. Genet. Couns. 2019 , 28 , 1098–1106. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Graetz, D.E.; Madni, A.; Gossett, J.; Kang, G.; Sabin, J.A.; Santana, V.M.; Russo, C.L. Role of Implicit Bias in Pediatric Cancer Clinical Trials and Enrollment Recommendations among Pediatric Oncology Providers. Cancer 2021 , 127 , 284–290. [ Google Scholar ] [ CrossRef ]
- Guedj, R.; Marini, M.; Kossowsky, J.; Berde, C.; Mateo, C.; Fleegler, E.W. Explicit and Implicit Bias Based on Race, Ethnicity, and Weight among Pediatric Emergency Physicians. Acad. Emerg. Med. 2021 , 28 , 1073–1076. [ Google Scholar ] [ CrossRef ]
- Guillermo, S.; Barre-Hemingway, M. Pain Perception and Treatment for Adolescents in Racially Concordant Versus Discordant Patient–Provider Scenarios. J. Adolesc. Health 2020 , 66 , 589–596. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hagiwara, N.; Penner, L.A.; Gonzalez, R.; Eggly, S.; Dovidio, J.F.; Gaertner, S.L.; West, T.; Albrecht, T.L. Racial Attitudes, Physician-Patient Talk Time Ratio, and Adherence in Racially Discordant Medical Interactions. Soc. Sci Med. 2013 , 87 , 123–131. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hagiwara, N.; Slatcher, R.B.; Eggly, S.; Penner, L.A. Physician Racial Bias and Word Use during Racially Discordant Medical Interactions. Health Commun. 2017 , 32 , 401–408. [ Google Scholar ] [ CrossRef ]
- Hagiwara, N.; Dovidio, J.F.; Eggly, S.; Penner, L.A. The Effects of Racial Attitudes on Affect and Engagement in Racially Discordant Medical Interactions between Non-Black Physicians and Black Patients. Group Process. Intergroup Relat. 2016 , 19 , 509–527. [ Google Scholar ] [ CrossRef ]
- Haider, A.H.; Schneider, E.B.; Sriram, N.; Dossick, D.S.; Scott, V.K.; Swoboda, S.M.; Losonczy, L.; Haut, E.R.; Efron, D.T.; Pronovost, P.J.; et al. Unconscious Race and Class Bias: Its Association with Decision Making by Trauma and Acute Care Surgeons. J. Trauma Acute Care Surg. 2014 , 77 , 409–416. [ Google Scholar ] [ CrossRef ]
- Haider, A.H.; Schneider, E.B.; Sriram, N.; Dossick, D.S.; Scott, V.K.; Swoboda, S.M.; Losonczy, L.; Haut, E.R.; Efron, D.T.; Pronovost, P.J.; et al. Unconscious Race and Social Class Bias among Acute Care Surgical Clinicians and Clinical Treatment Decisions. JAMA Surg. 2015 , 150 , 457–464. [ Google Scholar ] [ CrossRef ]
- Haider, A.H.; Schneider, E.B.; Sriram, N.; Scott, V.K.; Swoboda, S.M.; Zogg, C.K.; Dhiman, N.; Haut, E.R.; Efron, D.T.; Pronovost, P.J.; et al. Unconscious Race and Class Biases among Registered Nurses: Vignette-Based Study Using Implicit Association Testing. J. Am. Coll. Surg. 2015 , 220 , 1077–1086. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Halvorson, E.E.; Curley, T.; Wright, M.; Skelton, J.A. Weight Bias in Pediatric Inpatient Care. Acad. Pediatr. 2019 , 19 , 780–786. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hausmann, L.R.M.; Myaskovsky, L.; Niyonkuru, C.; Oyster, M.L.; Switzer, G.E.; Burkitt, K.H.; Fine, M.J.; Gao, S.; Boninger, M.L. Examining Implicit Bias of Physicians Who Care for Individuals with Spinal Cord Injury: A Pilot Study and Future Directions. J. Spinal Cord Med. 2015 , 38 , 102–110. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hirsh, A.T.; Hollingshead, N.A.; Ashburn-Nardo, L.; Kroenke, K. The Interaction of Patient Race, Provider Bias, and Clinical Ambiguity on Pain Management Decisions. J. Pain 2015 , 16 , 558–568. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hirsh, A.T.; Anastas, T.M.; Miller, M.M.; Quinn, P.D.; Kroenke, K. Patient Race and Opioid Misuse History Influence Provider Risk Perceptions for Future Opioid-Related Problems. Am. Psychol. 2020 , 75 , 784–795. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hirsh, A.T.; Hollingshead, N.A.; Matthias, M.S.; Bair, M.J.; Kroenke, K. The Influence of Patient Sex, Provider Sex, and Sexist Attitudes on Pain Treatment Decisions. J. Pain 2014 , 15 , 551–559. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hull, S.J.; Tessema, H.; Thuku, J.; Scott, R.K. Providers PrEP: Identifying Primary Health Care Providers’ Biases as Barriers to Provision of Equitable PrEP Services. J. Acquir. Immune Defic. Syndr. 2021 , 88 , 165–172. [ Google Scholar ] [ CrossRef ]
- Johnson, T.J.; Hickey, R.W.; Switzer, G.E.; Miller, E.; Winger, D.G.; Nguyen, M.; Saladino, R.A.; Hausmann, L.R.M. The Impact of Cognitive Stressors in the Emergency Department on Physician Implicit Racial Bias. Acad. Emerg. Med. 2016 , 23 , 297–305. [ Google Scholar ] [ CrossRef ]
- Johnson, T.J.; Winger, D.G.; Hickey, R.W.; Switzer, G.E.; Miller, E.; Nguyen, M.B.; Saladino, R.A.; Hausmann, L.R.M. Comparison of Physician Implicit Racial Bias Toward Adults Versus Children. Acad. Pediatr. 2017 , 17 , 120–126. [ Google Scholar ] [ CrossRef ]
- Lepièce, B.; Reynaert, C.; van Meerbeeck, P.; Lorant, V. General Practice and Ethnicity: An Experimental Study of Doctoring. BMC Fam. Pract. 2014 , 15 , 89. [ Google Scholar ] [ CrossRef ]
- Liang, J.; Wolsiefer, K.; Zestcott, C.A.; Chase, D.; Stone, J. Implicit Bias toward Cervical Cancer: Provider and Training Differences. Gynecol. Oncol. 2019 , 153 , 80–86. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Londono Tobon, A.; Flores, J.M.; Taylor, J.H.; Johnson, I.; Landeros-Weisenberger, A.; Aboiralor, O.; Avila-Quintero, V.J.; Bloch, M.H. Racial Implicit Associations in Psychiatric Diagnosis, Treatment, and Compliance Expectations. Acad. Psychiatry 2021 , 45 , 23–33. [ Google Scholar ] [ CrossRef ]
- Lowe, C.L.; Beach, M.C.; Roter, D.L. Genetic Counselor Implicit Bias and Its Effects on Cognitive and Affective Exchanges in Racially Discordant Simulations. J. Genet. Couns. 2020 , 29 , 332–341. [ Google Scholar ] [ CrossRef ]
- Nash, P.; Stuart-Hamilton, I.; Mayer, P. The Continuation of Prejudice: Addressing Negative Attitudes in Nurse Training and Continuing Professional Education. Educ. Gerontol. 2014 , 40 , 53–60. [ Google Scholar ] [ CrossRef ]
- Nymo, L.S.; Aabakken, L.; Lassen, K. Priority and Prejudice: Does Low Socioeconomic Status Bias Waiting Time for Endoscopy? A Blinded, Randomized Survey. Scand. J. Gastroenterol. 2018 , 53 , 621–625. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Oliver, M.N.; Wells, K.M.; Joy-Gaba, J.A.; Hawkins, C.B.; Nosek, B.A. Do Physicians’ Implicit Views of African Americans Affect Clinical Decision Making? J. Am. Board Fam Med. 2014 , 27 , 177–188. [ Google Scholar ] [ CrossRef ]
- Patel, N.; Patel, S.; Cotti, E.; Bardini, G.; Mannocci, F. Unconscious Racial Bias May Affect Dentists’ Clinical Decisions on Tooth Restorability: A Randomized Clinical Trial. JDR Clin. Transl. Res. 2019 , 4 , 19–28. [ Google Scholar ] [ CrossRef ]
- Penner, L.A.; Dovidio, J.F.; Gonzalez, R.; Albrecht, T.L.; Chapman, R.; Foster, T.; Harper, F.W.K.; Hagiwara, N.; Hamel, L.M.; Shields, A.F.; et al. The Effects of Oncologist Implicit Racial Bias in Racially Discordant Oncology Interactions. J. Clin. Oncol 2016 , 34 , 2874–2880. [ Google Scholar ] [ CrossRef ]
- Puumala, S.E.; Burgess, K.M.; Kharbanda, A.B.; Zook, H.G.; Castille, D.M.; Pickner, W.J.; Payne, N.R. The Role of Bias by Emergency Department Providers in Care for American Indian Children. Med. Care 2016 , 54 , 562–569. [ Google Scholar ] [ CrossRef ]
- Robstad, N.; Siebler, F.; Söderhamn, U.; Westergren, T.; Fegran, L. Design and Psychometric Testing of Instruments to Measure Qualified Intensive Care Nurses’ Attitudes toward Obese Intensive Care Patients. Res. Nurs. Health 2018 , 41 , 525–534. [ Google Scholar ] [ CrossRef ]
- Robstad, N.; Westergren, T.; Siebler, F.; Söderhamn, U.; Fegran, L. Intensive Care Nurses’ Implicit and Explicit Attitudes and Their Behavioural Intentions towards Obese Intensive Care Patients. J. Adv. Nurs. 2019 , 75 , 3631–3642. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rojas, M.; Walker-Descartes, I.; Laraque-Arena, D. An Experimental Study of Implicit Racial Bias in Recognition of Child Abuse. Am. J. Health Behav. 2017 , 41 , 358–367. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sabin, J.A.; Greenwald, A.G. The Influence of Implicit Bias on Treatment Recommendations for 4 Common Pediatric Conditions: Pain, Urinary Tract Infection, Attention Deficit Hyperactivity Disorder, and Asthma. Am. J. Public Health 2012 , 102 , 988–995. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sabin, J.A.; Marini, M.; Nosek, B.A. Implicit and Explicit Anti-Fat Bias among a Large Sample of Medical Doctors by BMI, Race/Ethnicity and Gender. PLoS ONE 2012 , 7 , e48448. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sabin, J.A.; Moore, K.; Noonan, C.; Lallemand, O.; Buchwald, D. Clinicians’ Implicit and Explicit Attitudes about Weight and Race and Treatment Approaches to Overweight for American Indian Children. Child. Obes. 2015 , 11 , 456–465. [ Google Scholar ] [ CrossRef ]
- Sabin, J.A.; Riskind, R.G.; Nosek, B.A. Health Care Providers’ Implicit and Explicit Attitudes toward Lesbian Women and Gay Men. Am. J. Public Health 2015 , 105 , 1831–1841. [ Google Scholar ] [ CrossRef ]
- Sandhu, H.S.; Arora, A.; Brasch, J.; Streiner, D.L. Mental Health Stigma: Explicit and Implicit Attitudes of Canadian Undergraduate Students, Medical School Students, and Psychiatrists. Can. J. Psychiatry 2019 , 64 , 209–217. [ Google Scholar ] [ CrossRef ]
- Schaa, K.L.; Roter, D.L.; Biesecker, B.B.; Cooper, L.A.; Erby, L.H. Genetic Counselors’ Implicit Racial Attitudes and Their Relationship to Communication. Health Psychol. 2015 , 34 , 111–119. [ Google Scholar ] [ CrossRef ]
- Schoenberg, E.; Wang, J.V.; Duffy, R.; Keller, M. Uncovering Unconscious Bias and Health Disparities in the Practice of Dermatology. Skinmed 2019 , 17 , 367–368. [ Google Scholar ]
- Schroyen, S.; Missotten, P.; Jerusalem, G.; Gilles, C.; Adam, S. Ageism and Caring Attitudes among Nurses in Oncology. Int. Psychogeriatr. 2016 , 28 , 749–757. [ Google Scholar ] [ CrossRef ]
- Setchell, J.; Watson, B.; Jones, L.; Gard, M.; Briffa, K. Physiotherapists Demonstrate Weight Stigma: A Cross-Sectional Survey of Australian Physiotherapists. J. Physiother. 2014 , 60 , 157–162. [ Google Scholar ] [ CrossRef ]
- Siegelman, J.N.; Woods, C.; Salhi, B.; Heron, S. Health Care Disparities Education Using the Implicit Association Test. Med. Educ. 2016 , 50 , 1158–1159. [ Google Scholar ] [ CrossRef ]
- Stepanikova, I. Racial-Ethnic Biases, Time Pressure, and Medical Decisions. J. Health Soc. Behav. 2012 , 53 , 329–343. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sukhera, J.; Wodzinski, M.; Teunissen, P.W.; Lingard, L.; Watling, C. Striving While Accepting: Exploring the Relationship Between Identity and Implicit Bias Recognition and Management. Acad. Med. 2018 , 93 , S82–S88. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tajeu, G.S.; Halanych, J.; Juarez, L.; Stone, J.; Stepanikova, I.; Green, A.; Cherrington, A.L. Exploring the Association of Healthcare Worker Race and Occupation with Implicit and Explicit Racial Bias. J. Natl Med. Assoc. 2018 , 110 , 464–472. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tucker Edmonds, B.; McKenzie, F.; Austgen, M.B.; Ashburn-Nardo, L.; Matthias, M.S.; Hirsh, A.T. Obstetrical Providers’ Management of Chronic Pain in Pregnancy: A Vignette Study. Pain Med. 2017 , 18 , 832–841. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- VanPuymbrouck, L.; Friedman, C.; Feldner, H. Explicit and Implicit Disability Attitudes of Healthcare Providers. Rehabil. Psychol. 2020 , 65 , 101–112. [ Google Scholar ] [ CrossRef ]
- Walden, T.A.; Lesner, T.A.; Jones, R.M. Is What I Think I Think Really What I Think? Implicit and Explicit Attitudes toward Stuttering among Practicing Speech-Language Pathologists. J. Commun. Disord. 2020 , 83 , 105965. [ Google Scholar ] [ CrossRef ]
- Wandner, L.D.; Heft, M.W.; Lok, B.C.; Hirsh, A.T.; George, S.Z.; Horgas, A.L.; Atchison, J.W.; Torres, C.A.; Robinson, M.E. The Impact of Patients’ Gender, Race, and Age on Health Care Professionals’ Pain Management Decisions: An Online Survey Using Virtual Human Technology. Int. J. Nurs. Stud. 2014 , 51 , 726–733. [ Google Scholar ] [ CrossRef ]
- Welch, L.C.; Lutfey, K.E.; Gerstenberger, E.; Grace, M. Gendered Uncertainty and Variation in Physicians’ Decisions for Coronary Heart Disease: The Double-Edged Sword of “Atypical Symptoms”. J. Health Soc. Behav. 2012 , 53 , 313–328. [ Google Scholar ] [ CrossRef ]
- Welch, L.C.; Litman, H.J.; Borba, C.P.C.; Vincenzi, B.; Henderson, D.C. Does a Physician’s Attitude toward a Patient with Mental Illness Affect Clinical Management of Diabetes? Results from a Mixed-Method Study. Health Serv. Res. 2015 , 50 , 998–1020. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wittlin, N.M.; Dovidio, J.F.; Burke, S.E.; Przedworski, J.M.; Herrin, J.; Dyrbye, L.; Onyeador, I.N.; Phelan, S.M.; van Ryn, M. Contact and Role Modeling Predict Bias against Lesbian and Gay Individuals among Early-Career Physicians: A Longitudinal Study. Soc. Sci Med. 2019 , 238 , 112422. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zestcott, C.A.; Spece, L.; McDermott, D.; Stone, J. Health Care Providers’ Negative Implicit Attitudes and Stereotypes of American Indians. J. Racial Ethn Health Disparities 2021 , 8 , 230–236. [ Google Scholar ] [ CrossRef ]
- IAT Corporation. Project Implicit. Available online: www.implicit.harvard.edu (accessed on 8 May 2023).
- Lee, D.J. Racial Bias and the Validity of the Implicit Association Test ; The United Nations University World Institute for Development Economics Research (UNU-WIDER): Helsinki, Finland, 2016. [ Google Scholar ] [ CrossRef ]
- Greenwald, A.G.; Poehlman, T.A.; Uhlmann, E.L.; Banaji, M.R. Understanding and Using the Implicit Association Test: III. Meta-Analysis of Predictive Validity. J. Pers. Soc. Psychol. 2009 , 97 , 17. [ Google Scholar ] [ CrossRef ]
- Karpinski, A.; Steinman, R.B.; Hilton, J.L. Attitude Importance as a Moderator of the Relationship between Implicit and Explicit Attitude Measures. Personal. Soc. Psychol. Bull. 2005 , 31 , 949–962. [ Google Scholar ] [ CrossRef ]
- Rezaei, A.R. Validity and Reliability of the IAT: Measuring Gender and Ethnic Stereotypes. Comput. Hum. Behav. 2011 , 27 , 1937–1941. [ Google Scholar ] [ CrossRef ]
- Meissner, F.; Grigutsch, L.A.; Koranyi, N.; Müller, F.; Rothermund, K. Predicting Behavior with Implicit Measures: Disillusioning Findings, Reasonable Explanations, and Sophisticated Solutions. Front. Psychol. 2019 , 10 , 2483. [ Google Scholar ] [ CrossRef ]
- Friese, M.; Hofmann, W.; Wänke, M. When Impulses Take over: Moderated Predictive Validity of Explicit and Implicit Attitude Measures in Predicting Food Choice and Consumption Behaviour. Br. J. Soc. Psychol. 2008 , 47 , 397–419. [ Google Scholar ] [ CrossRef ]
- Greenwald, A.G.; Nosek, B.A.; Banaji, M.R. Understanding and Using the Implicit Association Test: I. An Improved Scoring Algorithm. J. Personal. Soc. Psychol. 2003 , 85 , 197. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Bias | Number of Studies |
|---|---|
| Racial bias | 46 |
| Gender bias | 11 |
| Weight bias | 10 |
| SES bias | 9 |
| Mental illness bias | 7 |
| Disability bias | 7 |
| Ageism | 4 |
| LGBTQ bias | 2 |
| Diagnosis bias (cervical cancer) | 1 |
| Total | 97 |
| Country | Type of Bias | Number of Biases Assessed per Bias | Total Number of Biases Assessed per Country |
|---|---|---|---|
| Australia (n = 3) | Weight bias Mental illness bias | 2 1 | 3 |
| Belgium (n = 2) | Ageism Racial bias | 1 1 | 2 |
| Canada (n = 2) | Mental illness bias | 2 | 2 |
| Denmark (n = 1) | Weight bias | 1 | 1 |
| France (n = 1) | Disability bias | 1 | 1 |
| Italy (n = 2) | Disability bias Racial bias | 1 1 | 2 |
| Japan (n = 1) | Mental illness bias | 1 | 1 |
| Kenya (n = 1) | SES bias | 1 | 1 |
| Norway (n = 3) | Weight bias SES bias | 2 1 | 3 |
| Poland (n = 1) | Mental illness bias | 1 | 1 |
| Portugal (n = 1) | Gender bias | 1 | 1 |
| Saudia Arabia (n = 1) | SES bias | 1 | 1 |
| Sweden (n = 1) | Gender bias | 1 | 1 |
| UK (n = 1) | Ageism | 1 | 1 |
| USA (n = 58) | Racial bias | 44 | |
| Gender bias | 9 | ||
| SES bias | 6 | ||
| Weight bias | 4 | ||
| Disability bias | 4 | ||
| LGBTQ bias | 2 | ||
| Mental illness bias | 2 | ||
| Ageism | 2 | ||
| Diagnosis bias | 1 | 74 | |
| Global (n = 2) | Disability bias | 1 | |
| Weight bias | 1 | 2 |
| Bias | Number of Studies |
|---|---|
| Physicians | 51 |
| Nurses | 20 |
| Health care providers (not specified) | 12 |
| Psychiatrists | 5 |
| Dentists | 4 |
| Genetic counsellors | 4 |
| Physiotherapists | 3 |
| Mental health providers (not specified) | 2 |
| Physician assistants | 1 |
| Speech–language pathologists | 1 |
| Dieticians | 1 |
| Diagnostic radiographers | 1 |
| Occupational therapists | 1 |
| Midwives | 1 |
| Psychotherapists | 1 |
| Other support staff | 1 |
| Physicians | Nurses | Health Care Providers (Not Specified) | Dentists | Psychiatrists | Genetic Counselors | Physiotherapists | Rehabilitation Staff (Not Specified) | Physician Assistants | Mental Health Providers (Not Specified) | Dietitians | Occupational Therapists | Speech–Language Pathologists | Diagnostic Radiographers | Midwives | Psychotherapists | Other Support Staff | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Race | 34 | 8 | 6 | 2 | 1 | 2 | 1 | 1 | |||||||||
| Gender | 8 | 3 | 1 | 1 | 1 | ||||||||||||
| SES | 7 | 2 | 1 | 1 | 1 | ||||||||||||
| Weight | 5 | 4 | 1 | 1 | 1 | 1 | |||||||||||
| Mental illness | 3 | 1 | 4 | 1 | 1 | ||||||||||||
| Disability | 2 | 2 | 4 | 2 | 2 | 2 | 1 | 1 | |||||||||
| LGBTQ | 2 | 1 | 1 | 1 | |||||||||||||
| Ageism | 2 | 3 | 1 | ||||||||||||||
| Diagnosis | 1 | 1 | |||||||||||||||
| Total | 64 | 25 | 13 | 6 | 5 | 4 | 3 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Meidert, U.; Dönnges, G.; Bucher, T.; Wieber, F.; Gerber-Grote, A. Unconscious Bias among Health Professionals: A Scoping Review. Int. J. Environ. Res. Public Health 2023 , 20 , 6569. https://doi.org/10.3390/ijerph20166569
Meidert U, Dönnges G, Bucher T, Wieber F, Gerber-Grote A. Unconscious Bias among Health Professionals: A Scoping Review. International Journal of Environmental Research and Public Health . 2023; 20(16):6569. https://doi.org/10.3390/ijerph20166569
Meidert, Ursula, Godela Dönnges, Thomas Bucher, Frank Wieber, and Andreas Gerber-Grote. 2023. "Unconscious Bias among Health Professionals: A Scoping Review" International Journal of Environmental Research and Public Health 20, no. 16: 6569. https://doi.org/10.3390/ijerph20166569
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- English/Global
- Member Login

The Science of Unconscious Bias: What, Why, & How
by Michael Miller | Sep 4, 2018

A growing body of psychology research points to an uncomfortable truth about decision making: unconscious bias influences all of us and even the simplest decisions we make. Whether it’s our level of hunger, the time of day, or our mood, there are quite a few internal and external factors that creep into our decision making equation without our permission or awareness – and quite literally change our minds.
The research is equally amazing and alarming. If the people whose job it is to decide on inmates’ parole and students’ college admissions are biased by unrelated factors and they don’t even know it, how can we protect our own decisions from unwanted influence?
The first step is to understand the most common forms of bias that everyone experiences but hardly anyone recognizes. And the next step is to employ specific strategies to protect ourselves against making faulty, biased decisions unwittingly.
Let’s start by looking at the fascinating psychology research into unconscious bias that proves just how prevalent it is. Warning: it’s kind of scary.
Prisoners’ Parole Applications: A Shocking Example of Unconscious Bias

Are Israeli courtrooms biased against Palestinians? That’s one of many possibilities a team of researchers in Israel considered as they looked for patterns in the granting of parole. And they found a pattern all right, but not the one anyone expected. What made the biggest difference was the part of the session when the committees’ decided on each case. That’s right. The decision of whether someone should stay locked up, or go free, largely came down to a factor that had nothing to do with the case itself.
Let that marinade for a minute.
It’s pretty messed up, huh? I could hardly believe it. But it’s true. The committees were far less likely to grant parole toward the end of a session, most likely the result of what’s known as decision making fatigue. There are many factors that go into the decision of whether or not to grant parole; it’s a complex decision that takes into account the crime, time served, and other circumstances. As the session goes on and they hear multiple cases, the committee members get tired, and as they do, the fatigue makes them increasingly likely to stick with the status quo, which in this case meant denying parole applications. But this all happened without them knowing that anything but the facts at hand had influenced their decisions.
That’s unconscious bias at work.
You can read more about the research here.
A similar study in the United States found that the time of day when admissions officers read a high school applicants’ essay played an outsized role in how they scored it. It’s scary that a decision so important like a prisoner’s parole or a student’s college admission could be influenced by something so random, right? But that is the power of unconscious bias on decision making, and the same phenomenon impacts every one of us as we make all types of decisions. We’re often biased in ways that we’re not even aware of.
To understand the extent to which we are all biased, consider this study from the University of Virginia on hunger and visual perception. It turns out that what we see isn’t always very accurate.
Research finds evidence of unconscious bias in parole committees’ decision making – the time of day when the committees decided a case heavily influenced the outcome. Scary stuff, huh? And in terms of unconscious bias, this is just one study in a growing body of research…
How Big Is That Hill? Unconscious Bias and Getting Hangry

Imagine that you have a group of people at the bottom of a hill. If you came up with some way for them to describe the size of the hill, they would probably all say something similar, right? They are, after all, staring at the same exact hill, and it is a specific size. But actually that’s not how it works. Everyone’s perception of the hill is different based on the resources each person has to climb it at that moment.
In a research study at the University of Virginia, researchers divided participants into groups based on the amount of glucose they were given before rating the difficulty of climbing the hill. The presence or absence of glucose, a simple sugar and the body’s preferred fuel for physical exertion, determined how big the hill seemed for each person. The more glucose they had, the smaller the hill seemed. The less glucose, the bigger the hill. Now how could this be?
It really comes down to the fact that the brain is more concerned with survival than objectivity. To our brains, it’s less important how big the hill actually is and more important how big it is relative to our resources. On a very basic, biological level, we all experience the world through biased lenses. Our brains are biased to ensure our survival above all else, even the truth.
How big is that mountain? It depends on how hunger you are, according to research from the University of Virginia. Because the human brain is more concerned with surviving and thriving than it is with objectivity.
Research into hunger more generally has found that it tends to amplify the negativity of a negative experience. This is the experience commonly known as hanger – hunger driven anger. I’d speculate that the same forces are at play here. Since we have less resources to deal with the negative stimulus, it seems more overwhelming, and just plain worse.
And in a very similar way to the judges in Israel and the admissions officers in the US, the group at the bottom of the hill or someone who is hungry isn’t aware that the amount of glucose in their blood is impacting its perceptions of the world, and as a result, its decision making. But it is – in a very real, measurable way. That’s unconscious bias at work.
So fatigue and hunger are two forms of unconscious bias. And the last one I want to look at, and it’s probably the hardest to perceive and guard against because it’s changing all the time, is our mood.
You Don’t See That ? Unconscious Bias and Mood Goggles

Of all the stimulus that comes upon our eyes, ears and noses every day, we consciously take in about 1% of it. We’re always filtering; we have to. But the crazy part is, we tend to notice things that match the way we’re already feeling. Our brains like certainty, to know what’s going on. So when we’re anxious, we’re more likely to see threats. When we feel serene, we’re more likely to see evidence that the world is wonderful. The result is that the way we’re already feeling is reinforced – again and again. As I have struggled with depression over the years, I have felt the extreme of this tendency: When you are depressed, you see obstacles and hopelessness all around.
And what’s more is that these feelings, just like the physical sensation of hunger, impact our decision making in a big way. Fear breeds uncertainty and a limited perspective. Anger instills confidence and a greater tolerance for risk than normal. Sadness tends to make people more analytical. Even happiness has been found to make people more gullible. If we’re not aware of these biases, we can make some really suboptimal decisions. Our mood changes and we think, “Gee, why didn’t I analyze that more carefully? Or why did I over analyze that situation to death?”
Have you ever made a decision that you could clearly see in retrospect had been influenced by your mood? If so, share it in the comments below.
So considering all this, how can we be sure that we’re not making biased decisions?
Fascinating psychology research into unconscious bias, and 5 tips to increase self-awareness and check your own decisions for bias.
5 Ways to Overcome Unconscious Bias
Unconscious bias exists for all of us, so what can we do to overcome this limitation and make optimal decisions?
There is no surefire way, but here are 5 steps to go through and check for your own unconscious biases:
1. Check your basic needs. Am I hungry? Thirsty? Tired? Do I need to go to the bathroom? And you can not only think about if these things are true, but also think about how they would impact the decisions you’re making if they were. If I am hungry or tired, for instance, and a coworker asks me to take on an extra project, how would that influence my thinking as I go to respond? The answer to this one is clear: Hunger and fatigue mean that I don’t have the resources, and I would be more likely to decline or feel overwhelmed. Which is fine unless you think about how easy those are to change, and then I may want to hold off for a couple hours, or days, before responding. So be sure to check your basic needs before making almost any type of decision.
2. Take your emotional temperature. Ask yourself, what am I feeling? And how would that impact the decision I am making? Write down your feeling and compare it to the research on how that may influence your decision making progress. In today’s technological age, when sending what my Dad calls ‘email missiles’ is easier and more common than ever, this is a really vital skill. I am angry, and that could make me overconfident and minimize the risk I am taking by doing this. Or more often for me, I am sad and that could make me overanalyze a decision, even one as simple as how to word a text message. Recognizing these patterns before you make the decision is a game changer.
3. Consider big decisions in several sittings. Since fatigue, mood, hunger, the time of day, and even the lighting in a room have all been found to influence our decisions, it’s probably best to think about big decisions at several different times and in different locations. That way you can be sure that you are looking at it from several different angles, and sort of hedging your bets against making a biased decision.
4. Pretend to be someone else. A growing body of research shows that one way we’re unconsciously biased is in reserving wise reasoning for others’ problems that we do not apply to our own. It’s known as Solomon’s Paradox. For more on this, I highly recommend this article. To combat this trend, look at your own problems from a third-person perspective, like you are looking in on your own life. It may unearth some previously undiscovered biases in how you are thinking about the situation. For this to be effective, you should take care of you basic needs first, or you may think your friend’s situation is worse than it is!
5. Travel forward in time. Similarly, we often make decisions based on restraints and pressures related to time. So next time you are making a big decision, ask yourself: How would I feel about this in 5, 10 or 15 years? Thinking far into the future can help eliminate some unconscious bias and help us connect the decision to what really matters to us.
What’s new in emotional intelligence?

From Corporate Consultant to Coach: Elise Jones’ Emotional Intelligence Journey-Voices from the Network
Elise Jones transformed her career by embracing emotional intelligence, shifting from a corporate consultant to a passionate EQ Coach. Through authentic connections, she found deeper fulfilment, proving that strong relationships are key to a happier, more meaningful life.

Want to Manage Your Emotions More Effectively? Find Time to Journal About Challenging Experiences
Daily journaling to reframe unpleasant events can significantly reduce depressive symptoms, lessen stress, and increase life satisfaction.

A Journey through Empathy & Optimism: Amy Jimison in Voices from the Network
When you feel stuck and can’t see a way out, how do you navigate change? Certified Coach and leadership expert Amy Jimison shares her approach.
Trust, Diversity & Emotions: Key Strategies from EQ Diversity Practitioner Michael Eatman – Voices from the Network
Imagine a coaching client struggling with identity, belonging and diversity. How can you use emotional intelligence to help them build trust and overcome self-limiting beliefs to thrive?

Krish and Anabel: SEL Pioneer and Mentee Share 6 Life Lessons on Empathy, Integrity, and Emotional Intelligence
What are 6 life lessons you’ve learned? Dr. Anabel Jensen, SEL pioneer and Six Seconds President, explores this important question with her 16-year-old mentee.

Voices from the Network: Jeremy Jensen
In this Voices from the Network, we sit down with Police Chief Jeremy Jensen, who is doing emotional intelligence training with his officers in Dubuque, Iowa.
- Recent Posts
- Pursue Noble Goals in the Six Seconds Model of EQ - July 29, 2023
- Increase Empathy in the Six Seconds Model of EQ - July 26, 2023
- Exercise Optimism - July 24, 2023
Great article, Michael! This research dovetails beautifully with an area of great interest to me: law of attraction concepts and practices, through the unfolding of leading-edge discussions with Esther Abraham Hicks (via YouTube.) I love how this research underscores the understanding that we live in an attraction-based energetic universe, that like energies attract. It’s the how and the why we will always manifest experiences to reinforce our bias, our beliefs.
Every belief is a vibration. The question is, are we biased positively or negatively? And what is that positive or negative in relation to?
According to law of attraction principles, emotions fall on an energetic scale similar to frequencies on a radio tuner. Depression and despair at the bottom, appreciation and joy at the top. We are both the tuner of incoming radio frequencies–we receive frequencies–and we are transmitters, putting out vibrations. Most of the time unconsciously. And most of the time, we live in an echo chamber, receiving and transmitting back the conditions we perceive around us through our senses. Understood this way, emotions can be seen to serve as an internal guidance system to indicate being in alignment (+) or out of alignment/resistant (-).
The exciting thing: people are discovering we can learn to broadcast only the highest good, regardless of the conditions. And that is a big deal!
Picture a river flowing swiftly. Call it chi, ki, prana, grace, the eagle’s emanations, or all-that-is. When we are at the surface which is flowing 24/7 like a river, it feels good. Easy. Fun. Effortless. When we are out of alignment, we are resisting the current, and that feels bad. Like trying to swim upstream. Resistance is hard work. Resistance also pulls us down below the surface of stream, especially when we look backwards and hold on to grievances and fears. We get dragged right down towards the dark, resistant emotions.
When we are in a state of non-resistance, we float up like a cork, and become receivers of pure positive energy and a million cooperative components of the universe conspiring to help us. IT is because we have the leverage of the flow of source.
When we understand how law of attraction works, negative emotions become helpful indicators of misalignment, or resistance. We come to appreciate them as speed bumps at the edge of the highway. That appreciation itself brings us back up into alignment!
Negative emotions become not something to despair over, but valuable information to help us steer ourselves back up into the stream, in the flow. Becoming aware of and caring about our emotions, practicing shifting our emotional state deliberately to better-feeling, more positive vibrations, we can become conscious attractors, allowers, creators. That’s what law of attraction is all about.
This research also dovetails with all the great spiritual traditions as well. It explains why addicts hit rock bottom and then come back up: it is when we surrender, let go, trust, have faith, and release resistance — that we naturally float back up like corks, into the stream.
Reading this article, I feel quite heartened. Understanding from many different angles is coming to light at just the right time. As with all great advances throughout history, it is yet another turn of the upward spiral in the evolution in consciousness.
It has long been said that “hearts [emotions] that seek God [good] find him.” And that when one individual masters unconditional alignment with Source, they positively affect the vibration of 1,000 others around them. That would be interesting to study and document. I recently have been meeting people who are quite good at being in alignment unconditionally, and have witnessed their affect upon others.
Thanks for this article.
Great article, and resonates with me as a coach and teacher. When training teachers, I often recognise they are displaying unconscious bias that means their expectations of children and young people are limited. Developing their EQ can help them to recognise this and move towards adopting a more compassionate and egalitarian outlook for the children they teach.
That’s very interesting, Ruth. Thanks for sharing. A great coach can really help by making visible these forms of unconscious bias that are hard to see by oneself. What are the limiting beliefs that you often see teachers having about children?
It all starts with self awareness and ends with the choices we make. Great scientific insight very similar to the one practiced in CQ. EQ is so simple to understand, great to teach and hardest to apply. Yet, like life itself, it unravels only when we accept it.
Hi Rishabh,thanks for sharing. I agree that it all starts with self-awareness and acceptance, and really comes down to our choices. What is CQ?
Wonderful article with crucial insights for Self-Awareness and how it relates with our decision making. We really become a victim to our Unconscious Bias, especially in more demanding situations when we are challenged by mounting stress, hunger etc. Thanks Miller for bringing a very important aspect of decision making to our focus.
Thank you, Tauquir! You make a good point that unconscious bias and its effects seem to worsen – or sort of come to light – in demanding situations. As always, thanks for your support and insight!
Thanks for this important article. In these fractured times, disseminating the research is especially important!
No problem, Annette! I agree that it’s especially important these days. Thanks for reading and sharing!
Hi Annette, thank you! I enjoyed writing and sharing it, and you’re right, it’s very needed these days
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
This site uses Akismet to reduce spam. Learn how your comment data is processed .
"testing testing testing testing"
Not ready to buy your ticket for the EQ community event of the year? No problem! Sign up here and get this inside story on EQCON and all the developments
Workplaces that work for women
- Become a Supporter
- Our History
- Board of Directors
- Catalyst Staff
- Our Global Reach
- Board Directors Advisory Committee
- Catalyst CEO Champions For Change
- Expert Community
- Employee Resource Groups (ERGs)
- Measuring for Change
- Catalyst Partners
- Microlearning
- Learning Solutions
- Virtual Events
- Join Catalyst
- Attend Catalyst Honours
- Ask Catalyst
- Catalyst Awards
- More Solutions
Infographics
- Ask Catalyst Express
- Stats & Data
- Flip the Script
- Research Series
- Explore All Research
- Frontline Employees Initiative
- Remote Work
- Bias & Stereotypes
- Inclusive Future of Work
- Race, Ethnicity, and Culture
- Gender Partnership
- Pay Gap & Transparency
- More Topics
Content Type
- Biographies
- Spotlight Stories
- Media Releases
Research Type
- Infographic
- Session Recording
- Topic Overview
- Trend Brief
- Webinar Recording
- Allyship and Advocacy
- Artificial Intelligence
- Career Advancement
- DEI Governance
- DEI Messaging
- DEI Strategy
- Emotional Tax
- Employee Resource Groups
- Flexible Work
- Frontline Employees
- Gender Bias
- Gender Equity
- Gender Representation
- Inclusive Communications
- Inclusive Leadership
- Inclusive Workplaces
- Intersectionality
- Measurement
- Microaggressions
- Multigenerational Workplace
- Neurodiversity
- Organizational Culture Change
- Psychological Safety
- Recruitment and Retention
- Sexual Harassment
- Sponsorship and Mentoring
- Women of Color
- Women's Health
- Women's Workplace Health & Safety
- Workforce Trends
- Chinese (Simplified)
- Chinese (Traditional)
- Portuguese (Brazil)
- Latin America
- Middle East
- United States
Understanding Unconscious Bias: Ask Catalyst Express
Unconscious Bias is an association or attitude about a person or social group that, while not plainly expressed, operates beyond our control and awareness, informs our perceptions, and can influence our decision-making and behavior. It exists in each person’s worldview and affects our actions from the classroom to the workplace. And while we may not be conscious of our own biases, many of those around us do perceive them. As a result, unconscious bias creates barriers to inclusion, performance, engagement, and innovation. Though we cannot completely rid ourselves of unconscious bias, learning how to mitigate its impact is a skill that all of us can learn.
Catalyst Resources on Unconscious Bias
- 11 Harmful Types of Unconscious Bias and How to Interrupt Them
- 5 Ways to Identify Effective Unconscious Bias Training
- Artificial Intelligence: The New Frontier for Confronting Gender Bias
- Sharing Failures Leads to Learning Opportunities for All
- Boston Scientific: Accelerating Progress for Women by Creating Equal Opportunities for Growth Supporter Exclusive To reach an even wider audience, Boston Scientific instituted a required online unconscious bias training—available in 18 languages—to help employees reflect and recognize their own biases and embrace DEI efforts. To date, 98.6% of employees have completed this training. The company also created an online Inclusion Toolkit that offers employees on-demand content, including an inclusive behaviors self-assessment, manager skill-building resources, and educational anti-racism resources.
- Parexel: Leveraging Gender Partnership to Advance Women in Leadership Supporter Exclusive The first step was to educate leadership in such a way that they would feel personally committed to making this change—by sitting across the table and telling them that their unconscious bias was impacting the company’s ability to benefit from the contributions of many highly-qualified candidates. DEI leadership arranged a series of talks from outside speakers and invited senior leaders to attend; this effectively constituted some of the company’s first unconscious bias and inclusion training.
- The Boston Consulting Group (BCG)—Women@BCG Supporter Exclusive BCG also implemented many programs and activities that promote awareness and affiliation, including Unconscious Bias training that was mandatory for all Partners and Principals, as well as leaders who managed key people processes (such as recruitment and learning and development). Over 90% of Partners, Principals, leaders, and teams participated.
- Break the Cycle—Eliminating Gender Bias in Talent Management Systems ( see also: French translation )
- How to Combat Unconscious Bias as an Individual ( see also: French translation , Japanese translation )
- How to Combat Unconscious Bias as a Leader in Your Organization ( see also: French translation , Japanese translation )
- What is Unconscious Bias?
Online Learning
- CatalystX Discussion Facilitation Guide–Unconscious Bias: From Awareness to Action Supporter Exclusive
- Knowledge Burst: Running More Inclusive Meetings Supporter Exclusive
- Knowledge Burst: Managing Affinity Bias Supporter Exclusive
- Building Inclusion for Indigenous Peoples in Canadian Workplaces
- The Day-to-Day Experiences of Workplace Inclusion and Exclusion
- Day-to-Day Experiences of Emotional Tax Among Women and Men of Color in the Workplace
- Empowering Workplaces Combat Emotional Tax for People of Colour in Canada
- Engaging Men: Barriers and Gender Norms
- Break the Cycle—HR Experts: Eliminate Gender Bias From the Recruitment Process
- Break the Cycle—Managers: Eliminate Gender Bias in Development Opportunities
- Break the Cycle—Senior Leaders: Self-Assessment and Action Plan

Trend Briefs
- AI and Gender Bias
- Gendered Ageism
- A Conversation on Unconscious Bias Supporter Exclusive
- Eliminating the Double Bind Supporter Exclusive
- International Women’s Day – Sharing Perspectives (EMEA Roundtable Recording) Supporter Exclusive
Other Resources on Unconscious Bias
- Unconscious Bias, Implicit Bias, and Microaggressions: What Can We Do About Them? American Bar Association
- The Unconscious Bias in HR Series – #1. Introduction EuroGender
- How to Tackle Unconscious Bias in Your Workplace Forbes
- What Unconscious Bias Training Gets Wrong… And How to Fix It The Guardian
- Are You Aware of Your Biases? Harvard Business Review
- Test Yourself for Hidden Bias Learning for Justice
Return to Ask Catalyst Express .
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Implicit bias.
Harini S. Shah ; Julie Bohlen .
Affiliations
Last Update: March 4, 2023 .
- Continuing Education Activity
Implicit bias is the attitude or internalized stereotypes that unconsciously affect our perceptions, actions, and decisions. These unconscious biases often affect behavior that leads to unequal treatment of people based on race, ethnicity, gender identity, sexual orientation, age, disability, health status, and other characteristics. In medicine, unconscious bias-based discriminatory practices negatively impact patient care and medical training programs, hinder effective communication, limit workforce diversity, lead to inequitable distribution of research funding, impede career advancement, and result in carriers and disparities in the access to and delivery of healthcare services. This activity will address strategies to reduce the harm of implicit bias, clinician self-awareness and self-assessment of personal biases, and the role of the interprofessional team in increasing awareness and reducing bias-based discriminatory behavior.
- Recognize how implicit bias affects the perceptions and treatment decisions of clinicians leading to disparities in healthcare delivery and health outcomes.
- Identify stigmatized groups and strategies to eliminate discriminatory behavior in healthcare delivery for these groups.
- Describe strategies to increase awareness of personal unconscious biases in daily interactions and change behavior accordingly.
- Discuss how interdisciplinary teams can reduce the harmful effects of implicit bias in medicine.
- Introduction
Implicit biases are subconscious associations between two disparate attributes that can result in inequitable decisions. They operationalize throughout the healthcare ecosystem, impacting patients, clinicians, administrators, faculty, and staff. No individual is immune from the harmful effects of implicit biases. Unconscious bias-based discriminatory practices negatively impact patient care, medical training programs, hiring decisions, and financial award decisions and also limit workforce diversity, lead to inequitable distribution of research funding, and can impede career advancement. [1]
When implicit biases are ignored, they jeopardize delivering high-quality healthcare services. [2] A simple analogy can exemplify implicit bias in healthcare in action. Several physicians are reviewing the chest x-ray of a black man with a productive cough to determine a possible diagnosis. Another physician, not privy to the patient's demographics, joins the discussion later and quickly states that his condition most likely is cystic fibrosis. The clinicians were initially influenced by the patient's demographics and then realized the chest X-ray findings were diagnostic for late-stage cystic fibrosis, a condition more common in White populations than other races.
Explicit versus Implicit Bias
With explicit bias, individuals are aware of their negative attitudes or prejudices toward groups of people and may allow those attitudes to affect their behavior. The preference for a particular group is conscious. For example, a hospital CEO may seek a male physician to head a department due to his explicit belief that men make better leaders than women. This type of bias is fully conscious.
Implicit bias includes the subconscious feelings, attitudes, prejudices, and stereotypes an individual has developed due to prior influences and imprints throughout their lives. Individuals are unaware that subconscious perceptions, instead of facts and observations, affect their decision-making. Implicit bias and explicit bias are both problematic because they lead to discriminatory behavior and potentially suboptimal healthcare delivery.
We all hold implicit biases. Implicit bias is challenging to recognize in oneself; awareness of bias is one step toward changing one's behavior. [1] Cultural safety refers to the need for healthcare professionals to examine themselves and the potential impact of their culture, power, privilege, and personal biases on clinical interactions and healthcare delivery. This requires health providers to question their own attitudes, assumptions, stereotypes, and prejudices that may contribute to a lower quality of healthcare for some patients. Cultural safety compels healthcare professionals and organizations to engage in ongoing self-reflection and self-awareness and hold themselves accountable to provide culturally safe care, which the patients and their communities define. [3] Healthcare professionals and their healthcare organizations should work together to develop strategies to mitigate the harmful effects of bias and reduce bias-based decisions that contribute to barriers to healthcare access, healthcare disparities in patient care delivery, and lack of workforce diversity.
Stigmatized Groups and the Implicit Association Test (IAT)
Although we may consciously reject negative associations with stigmatized groups, it is virtually impossible to dissociate from a culture impregnated with such stereotypes. Patients from stigmatized groups may have one or more of these characteristics or conditions: advanced age, non-White race, HIV, disabilities, and substance or alcohol use disorders. [4] [5] [6] Other factors include low socioeconomic status, mental illness, non-English speaking, non-heterosexual, and obesity. [7] [8] [9] [10] Implicit biases, by definition, occur in the absence of salient understanding or conscious awareness. [11] [12] However, we can apply harm mitigation strategies to avoid the destructive implications of implicit bias. To this end, recognition is the first step.
Implicit biases in healthcare are well-characterized by studies that use Implicit Association Tests (IAT) to evaluate medical decision-making toward stigmatized groups. The IAT measures the strength of associations between concepts and evaluations or stereotypes to reveal an individual's hidden or subconscious biases (Project Implicit - implicit.harvard.edu). The IAT is a highly validated measure for implicit biases; although vulnerable to voluntary control, the tool remains a gold standard in implicit bias research. [13] [14] Studies have shown that strong implicit biases hinder communication. [15] Effective patient-healthcare provider (HCP) communication is associated with reduced patient morbidity and mortality, lower healthcare costs, and decreased rates of HCP burnout. [16] [17] [18] [16]
Implicit biases become destructive when they translate into microaggressions, defined as verbal or nonverbal cues that communicate hostile attitudes towards those from stigmatized groups. [19] [20] Although often unintentional, microaggressions maintain power structures and threaten the psychological safety of patients, resulting in adverse public health implications. [21] Reducing microaggressions has been shown to reduce HCP burnout and depression. [22] [23]
Implicit Bias Awareness and Training
Comprehensive implicit bias training enhances the healthcare workforce's financial value, productivity, and longevity. The recognition of implicit bias is the first step in mitigating its effects. Many states in the US require implicit bias training for employment and licensure in the healthcare profession. The ongoing engagement of implicit biases among HCPs promotes cultural safety in healthcare organizations, representing a critical consciousness that welcomes accountability in the collaborative effort to provide culturally safe healthcare as defined by patients and their communities. HCPs should be aware of their implicit biases but not blame themselves when situations out of their control arise—respect for themselves, peers, and patients is the utmost priority. Progress toward reducing implicit bias is limited without personal discomfort and vulnerability.
Currently, very limited knowledge exists on how to conduct effective implicit bias training. However, studies show that incorporating mindfulness, coalition-building, and personal retrospection alongside broader structural changes is integral in reducing the harmful effects of implicit bias in the clinical environment. [2] [24] [25] This article provides strategies to mitigate the impact of implicit biases among physicians, residents, physician assistants, pharmacists, registered nurses, nurse practitioners, medical assistants, medical scribes, certified registered nurse anesthetists, physical and occupational therapists, chiropractors, dentists, hygienists, licensed nutritionists, dieticians, social workers, counselors, psychologists, other allied health professionals, and healthcare trainees. Implicit bias in continuing education is required in many states.
Implicit Bias Training: State Legislation and Requirements for Healthcare Providers
California - AB241 (legislation)
Illinois - Sec. 2105-15.7 (legislation)
Michigan - R 338.7001 (legislation)
Maryland - HB28. Sec. 1-225 (legislation) (HB28)
Minnesota - Sec. 144.1461 (legislation)
Washington - Sec. 43.70.613 (legislation)
Massachusetts - 243 CMR 2.06(a)3 (legislation)
New York - S3077 (legislation)
Pennsylvania - HB 2110. Title 63. Sec. 2102a (legislation)
Indiana - HB 1178 (legislation)
Oklahoma - HB 2730 (legislation)
South Carolina - H 4712. Session 123 (legislation)
Tennessee - SB0956 and HB0642 (legislation)
- Issues of Concern
Harm-Reduction Strategies for Stigmatized Groups
Studies show that implicit bias training has little to no benefit without disaggregating the experiences of stigmatized groups and providing actionable recommendations. Here, we outline harm-reduction strategies, disaggregated based on the previously stigmatized groups (advanced age, nonwhite race, HIV positive, disabilities, substance use disorder, alcohol use disorder, low socioeconomic status, mental illness, non-English speaking, non-heterosexual, and obesity). Patients often belong to more than one group, given the intersectionality of historically disadvantaged populations in the US (e.g., being black with low socioeconomic status).
Persons of Advanced Age
Older adults are often associated with a cultural fear of death and dying. [26] [27] This fear is so pervasive that older adults may even internalize that they're a burden to others. [28] [21] HCPs may perceive older adults as less independent (regardless of decision-making capacity), attention-seeking, unrewarding to care for, and visually unpleasant. [29] From a mental health standpoint, physicians are less willing to treat older adults with suicidal ideation than young adults with suicidal ideation. Healthcare trainees are more comfortable interacting with older adults (compared to younger adults) with suicidal ideation. [30] Nurses with negative perceptions towards older adults provide less health education and have shorter patient interactions with older adults. [30]
Implicit bias can result in less mental health treatment for individuals of advanced age. Strategies to reduce implicit bias are created to educate clinicians that older adults deserve mental health treatment and should not be overlooked due to unconscious prejudicial negative feelings that clinicians may hold. HCPs should aim to schedule multiple health appointments in the same location and allot extra time for care for older adults. A healthcare team must ask for written permission before speaking with family members and caregivers. Healthcare teams should talk directly to patients even if a caregiver is present. Studies have shown that peer mentor support among older adults and support from those who have experienced illness facilitates patient empowerment. [31] Providing multiple forms of accessible communication ensures a complete understanding of care. [32]
Persons of Nonwhite Race
In 2021, the Center for Disease Control and Prevention (CDC) cited racism as a serious public health threat (CDC, 2021). Indeed, numerous studies have shown specific examples of race-based discrimination in healthcare settings. For example, implicit racial biases impact clinical decision-making for pain management, noninvasive cardiac testing, thrombolysis, cardiac catheterization, and cancer screening. [33] [21] Pediatric nonwhite patients also face implicit racial biases from HCPs. [34] [35] [36] Black, Latinx, and indigenous patients are frequently met with verbal dominance from HCPs and negative experiences in the medical setting, compromising trust in HCPs and patient care quality. [37] [38] [39] HCPs who score highly on the IAT for black-white implicit bias are often rated poorly by black patients regarding patient-centered care. [37] Implicit biases against those of nonwhite race are particularly salient when the clinician perceives increased time pressure and ambiguity, such as in acute care or emergencies. [40] [41] [42] The COVID-19 pandemic exacerbated discriminatory attitudes towards HCPs of Asian and Pacific Islander descent. [43] [44]
Strategies to reduce harm from implicit racial bias include finding things in common such as a shared group membership, which has been associated with a decrease in implicit racial bias. [25] Counter-stereotypical examples, such as a 36-year-old black male CEO of a Fortune 500 company, may also result in unconscious prejudice or stereotyping. [45] Expanding one's network and forming friendships with people of different healthcare professions further reduces the effect of implicit bias in the healthcare setting. [45] One may learn to recognize personal changes in non-verbal (e.g., gestures, eye contact, body distance) and paraverbal (e.g., tone, pitch, volume) communication behaviors. [46] [45] [21] Racialized experiences are valuable in a patient's health history; rather than ignoring these experiences, one can recognize their impact on health outcomes. HCPs may ask clinical questions to ascertain a patient's experiences with racism. [47] Examples of questions to determine racialized experiences are as follows:
- "Many of our patients face racism in healthcare; is this something you've experienced before?"
- "Are there any important life events that you've experienced or are currently experiencing that affect your health?"
Finally, it is essential to thank patients for sharing their stories, validate them, and acknowledge the trauma that those experiences may have caused. Knowledge of these experiences gives context to patients who lost trust in the healthcare system or may appear "non-compliant." Incorporating this practice into healthcare workflows enhances value-based care. [48]
Persons with Limited English Proficiency
The nature of implicit bias toward those with limited English proficiency stems from an inherent miscommunication in health care. For English speakers, speaking English in the work setting is comfortable; when HCPs are displaced from their comfort zone, study findings reveal that healthcare quality declines. The widespread use of medical interpreters has reduced many patient barriers, but interpreters are usually only available in large healthcare systems and are not often used during outpatient care. As a result, HCPs often translate to the best of their ability when communicating with a patient with limited English proficiency. Although faster, this method leaves wide gaps in the exchange of health information and treatment compliance. [49] [50] [51] As mentioned previously, patient unfamiliarity and HCP time constraints are two competing factors that widen disparities in healthcare delivery. [15]
Strategies to reduce harm due to implicit bias against those with limited English proficiency include consistently using professional medical translators in outpatient and inpatient settings. Before patient care visits, it is more effective if HCPs and staff can ensure the professional translator is available for the entire appointment. [15] Caution must be taken when caregivers or family members offer to translate for older adults, as studies show this approach compromises patient autonomy over their care.
Persons Living with HIV (PLWH)
The nature of implicit bias against persons living with HIV (PLWH) has deep roots in AIDS exceptionalism, a Western response to a lethal virus that initially disproportionately affected men who had sex with men (MSM). Fear and stigma in the early 1980s drove a public health response that worsened the alienation of PLWH. The long-term impact of this public health response is a deeply held, false narrative that PLWH are dangerous. This narrative continues to dampen opportunities for well-studied public health measures to expand prophylaxis, diagnosis, and treatment of HIV. [52]
Implicit biases and stigma associated with HIV are independent barriers to testing, adherence, and retention. [53] [54] HCPs are responsible for understanding their implicit biases against PLWH and reducing their influence on providing equitable, timely HIV treatment. Unlike other groups, greater exposure to PLWH and training to reduce the stigma associated with HIV is associated with more positive experiences among patients and HCPs. [55] Examples of implicit biases or perceptions held by HCPs are as follows: PLWH are poor, have many sexual partners, could have avoided HIV if they wanted to, and are affected due to risky or irresponsible behavior. [56] [57] Some studies have shown that HCPs would themselves feel ashamed if they were infected with HIV, contributing to a fear of occupational exposure to HIV. [55] [58] [59]
Strategies to reduce harm due to implicit biases against PLWH include actively countering the belief that HIV is avoidable without irresponsible behavior. Decades of studies have shown that PLWH is not the problem; a nationwide response that fails to protect its vulnerable population(s) has a more catastrophic outcome than the role of any individual group. [59] Furthermore, one must actively avoid the assumption that HIV runs in specific circles or neighborhoods; public health efforts to target at-risk groups do not necessarily equate to deeming which are high-risk communities.
Persons of the LGBTQIA+ Community
The stigma surrounding PLWH and its misconstrued association with the lesbian, gay, bisexual, transgender, or queer/questioning (LGBTQ) community is exacerbated by heteronormative microaggressions when receiving healthcare, conveying the message that non-heterosexual identities are abnormal, different, or inferior to the heterosexual majority. [60] Unsurprisingly, HCPs identifying as heterosexual tend to harbor these implicit associations. [61] [62] Among HCPs, mental health providers are least likely, and nurses are most likely to hold implicit preferences for heterosexual patients. [61] When caring for sexual minority patients, HCPs with implicit biases express discomfort while taking patient sexual histories and advising about safe sex behaviors, compromising the quality of care for sexual minority patients. [61]
To reduce harm from implicit biases against those identifying with the LGBTQ community, it is essential to do one's diligence in understanding the terminology and how patients define themselves. [63] For example, a person whose gender differs from that assigned at birth may refer to themselves as transsexual in formal settings but may also use self-descriptors such as trans, gender non-conforming, they/them/theirs, or nonbinary. HCPs should discuss and use patient self-descriptors both in communication and medical documentation. The more HCPs deliberately create safe spaces for patients of the LGBTQ community, the easier it will be to use patient self-descriptors in HCP workflows. [64]
Although not enough to produce culturally competent care, small changes such as supporting the observance of LGBTQ Pride Day or encouraging employees to use their descriptor pronouns can have a positive impact. [65] Lastly, HCPs should be aware of this population's relevant social and health needs and provide appropriate screenings and treatment without isolating patients. [66] Examples of these needs include violence prevention, comprehensive mental health treatment, discussions on substance and alcohol use, HPV screening, food insecurity, transgender transitional care, and hormonal therapy. [67] [68] [69] [70] [71]
Persons with Substance Use Disorder, Alcohol Use Disorder, History of Incarceration, or Exposure to Police Violence
Individuals with substance and alcohol use disorders, a history of incarceration, or exposure to police violence represent a population with significant unmet social and health needs. These unmet needs are exacerbated when HCPs hold negative implicit attitudes that individuals belonging to these groups are poorly motivated, manipulative, noncompliant, and violent. [72] [73] [74] HCPs have been shown to unfairly judge patient "treatability" before admission to rehabilitation programs, provide lower-quality palliative care for late-stage patients with cancer and substance use disorders and display microaggressions towards pregnant patients with substance use disorders during prenatal visits. [75] [76] [75] [77]
Studies findings reveal that medical, nursing, and pharmacy trainees rarely receive training in healthcare delivery for persons with histories of criminal legal system exposure, characterized as those with frequent police stops, arrests, and incarceration, despite this group representing 57% of men and 31% of women in the US population. [78] [79] [80] As more individuals are released from jails and prisons into the community, HCPs unaware of their prejudicial negative feelings toward persons with criminal legal system involvement may threaten the psychological safety of an already vulnerable, community-dwelling population. [81]
One goal of implicit bias awareness and training is to reduce the harmful effects of implicit biases toward community-dwelling persons with a history of criminal legal system involvement. To do this, we must first dismantle the idea that a person with a history of incarceration must be a bad person; some groups are more likely to be incarcerated due to race alone. [82] [83] Nearly 1 in 3 black men will be imprisoned in the US. [83] Furthermore, sentence length, police brutality, and delayed parole are features encumbered by implicit bias. [84] [85] [86] [87] Prevalent comorbidities such as severe mental illness make it virtually impossible to re-integrate into one's community without the assistance of a strong family network, healing environments, and financial resources. [88] [89] [90] Trauma-informed healthcare is messy, difficult, and time-consuming, but essential, given the complex health needs of this population. Individuals with a history of incarceration may present anywhere in the healthcare system. HCPs, when able, must carefully document these experiences in a protected health record to inform other HCPs and avoid re-traumatizing patients.
Persons with Low Socioeconomic Status or a History of Homelessness
It is well-documented that HCPs working in safety-net hospitals and emergency departments express disdain towards individuals with low socioeconomic status and homelessness, colloquially known as the "revolving door" of acute care utilization in this population. [91] [92] HCPs may perceive hospital admissions of patients with a history of homelessness as an unnecessary use of resources that may otherwise be used for those who need them. [93] [94] [95] Discriminatory behavior towards those experiencing homelessness is associated with suboptimal healthcare delivery and increased hospitalizations, exacerbating the "revolving door" problem. [54] [96] [97] [98] [99] [100] An explanation for discriminatory behavior among HCPs is relative exhaustion from large patient loads, administrative pushback, and competing demands in acute care environments, which tend to amplify implicit biases. [42] [41]
Strategies to reduce harm from implicit biases towards individuals from this group are twofold: 1) countering burnout with mindfulness and positive coping mechanisms and 2) eliminating the belief that low socioeconomic status and/or homelessness is earned. [101] [102] [103] [104] On the contrary, decades of research suggest that homelessness is neither incidental nor self-directed. Adverse childhood experiences and "poverty traps"—systems designed to siphon wealth from the poor to the wealthy—make it virtually impossible for those in poverty to gain enough social capital to access outpatient preventive healthcare. [105] [106] [107] Indeed, it may be easy to blame patients experiencing homelessness for their unmet health needs, but the habit of doing so perpetuates negative behaviors, worsens burnout, and decreases job satisfaction among HCPs. [108] [109] [110] [111]
Persons with a Disability
Evidence exists for the presence of implicit bias toward persons with a disability (PWD) from OT/PT specialists, [112] genetic counselors, [113] healthcare researchers, and other HCPs [114] [115] In the US, PWD receive suboptimal preventive care and have overall poorer health statuses compared to those without a disability, partly due to negative implicit attitudes from HCPs. [116] [117] [118] [119] When asked about their willingness to treat PWD, HCPs feel largely unprepared to care for PWD and prefer not to treat them due to limited education on PWD's unique health needs. [120] Interestingly, studies show that current healthcare education paradoxically promotes ableist viewpoints. [121] [120] [122]
To reduce harm from HCP implicit biases toward PWD, HCPs should involve PWD in redesigning clinic spaces to improve accessibility. Many US outpatient clinics have incorporated features such as wheelchair-accessible doors, touchscreens, height-adjustable exam tables, and scales with handrails, but the lack of national standardization remains a limitation. [123] [124] [125] Additionally, not including PWD in clinic redesign has led to mediocre improvements in accessibility. [125] [123] To address this issue, focus groups with PWD as team members could develop patient-centered questions to identify patients needing healthcare accommodations. [126] Long-term changes include increasing the representation of HCPs with disabilities. [127]
Persons with Mental Illness
The prevalence of mental illness is rising due to increased recognition and treatment (National Institute of Mental Health, 2022). Unfortunately, the negative stigma of having a mental illness prohibits many from seeking treatment. [21] [128] The stigma surrounding mental illness has deep roots in US history; in the 19th and early 20th centuries, those with severe mental illness were held in asylums with limited access to the outside world. Deinstitutionalization, or the release of patients with serious mental illness into the community, began in the 1950s and was largely driven by financial burdens for the rising welfare state in maintaining asylums. [129] [130] Unfortunately, closing asylums was not met with increased community-based mental health services, leading to the systematic stigmatization and criminalization of patients with serious mental illness. [129] This history reflects a broader message that forms implicit biases among HCPs today: that having a mental illness is shameful. [128] [131] [132] [21]
Strategies to reduce harm due to implicit biases toward those with mental illness include speaking up when HCP colleagues dismiss a patient's mental illness or use it as a reason for lower-quality medical treatment. [133] [134] [135] HCPs should avoid the assumption that patients with mental illness seek to take advantage of the healthcare system. [135] Indeed, numerous studies suggest that those with mental illness are quickly labeled as "frequent flyers" in acute care settings, more likely to be dismissed when complaining of pain, despite having more complex health needs. [136]
Persons with Obesity
Those with obesity are too often misrepresented as lazy, irresponsible, and lacking self-discipline; however, ample evidence suggests that genetic factors, socioeconomic status, and environment can change a person's obesity risk. [137] The idea that individuals with obesity are inferior is perpetuated in social media, colleges, and health care. [138]
Strategies to reduce harm to those with obesity starts with using appropriate terminology. For example, HCPs must use the word obesity as a noun describing an illness and not use the word obese as an adjective to describe a patient. The proper terminology is a patient with obesity and not an obese patient. This concept also applies to electronic health documentation; for example, the HCP should record a patient's information as a "31-year-old patient with obesity" and not a "31-year-old obese patient." [139] While HCPs must provide optimal health recommendations for patients, they must recognize the genetic, environmental, and ethnic factors influencing body fat distribution. The best outcomes for weight management occur in collaboration with an interdisciplinary team of dieticians, primary care providers, and bariatric services. [140]
- Clinical Significance
The US healthcare system poses many challenges to HCPs: administrative burden, high patient load, and inefficiencies. Acknowledging and reducing implicit biases may seem like insurmountable tasks given these challenges. After all, how can you be emotionally available to recognize your own biases when you are barely managing to keep the ship afloat? A part of this reality is true; it is impossible to eliminate one’s own implicit biases and treat everyone equally all the time. However, studies have shown that practicing mindfulness, attentional control, and emotional regulation, in addition to showing compassion when able, positively impacts the culture of healthcare. [54]
At the health systems level, providing implicit bias training courses for employees is not enough. Healthcare systems must 1) create stress-free spaces for HCPs to debrief and reflect on their experiences with implicit bias, 2) stop pressuring HCPs to constantly make major decisions during intense cognitive stress, and 3) provide opportunities for role-playing encounters with patients when implicit bias is perceived or acknowledged, as studies show the more HCPs practice these discussions, the more likely implicit biases are acknowledged and reflected upon in patient rooms. [9]
- Enhancing Healthcare Team Outcomes
Although the relationship between implicit bias and interdisciplinary teams is relatively unexplored, it is evident that no single member is responsible for molding a healthcare team's culture. A culture that values open discussion of biases and protects psychological safety promotes team productivity, whereas rudeness and negative behaviors in healthcare teams may adversely affect team performance. [141] [Level 1] The "butterfly effect" is the idea that small team changes can significantly impact other parts of the process or system; it occurs in a system where implicit biases are openly recognized without repercussions. [142] [Level 3]
Tools for self-reflection of implicit biases among healthcare teams have been shown to improve patient trust in the quality of care. [Level 1] Clear communication of expectations and responsibilities minimizes the impact of bias on choosing team roles. [143] [Level 1] Implicit bias training can provide new team knowledge when additional learning is needed. Graduate medical education that includes implicit bias training has been shown to improve leadership qualities in trainees, which may foster an equitable team culture. [144] [Level 1] However, isolated training does not result in equitable care without team members applying knowledge acquired in daily interactions. [1] [Level 3] Therefore, regular check-ins and debriefs are essential to ensuring that team members feel prepared to engage in self-improvement. [143] [Level 1]
Interprofessional Education Collaborative and Core Competencies
Interprofessional teams share their values, perspectives, and strategies for planning interventions, and each member of the team plays a role in delivering patient care. Team members share their expertise and skills to provide effective patient care and achieve optimal outcomes. Teams function optimally when the members effectively communicate and have mutual respect for each other and their individual roles. Four core competencies have been established for interprofessional collaborative practice (see IPEC Core Competencies for Interprofessional Education Collaborative):
- Work with individuals of other professions to maintain a climate of mutual respect and shared values. (Values/Ethics). When team members place a high value on treating patients and team members equally and respectfully and operate ethically, interventions to reduce the harmful effects of implicit bias that result in health disparities can be created in a culturally safe and accepting environment.
- Use the knowledge of one's own role and those of other professions to appropriately assess and address the health care needs of patients to promote and advance the health of populations. (Roles/Responsibilities) Each interprofessional team member is responsible for identifying how implicit bias affects perceptions and clinicians' treatment decisions, leading to disparities in healthcare delivery and health outcomes.
- Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to promoting and maintaining health and preventing and treating disease. (Interprofessional Communication) Discussions regarding cultural safety and the continued need for clinicians to engage in ongoing self-reflection and self-awareness and hold themselves accountable to provide culturally safe care should be a priority. Open discussions focused on accepting that everyone has implicit biases and that everyone has the ability to recognize them and change their behavior through interventions, such as counter-stereotyping, are helpful. Strategies to improve patient-clinician communication are beneficial, especially with patients in stigmatized groups.
- Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles to plan, deliver, and evaluate patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable (Teams and Teamwork) Teams should work together to develop strategies to eliminate discriminatory practices that result in disparities in healthcare delivery, limited access, and suboptimal patient outcomes. Time should be given to interventions that embrace and increase diversity in the workforce.
- Nursing, Allied Health, and Interprofessional Team Interventions
If members of an interprofessional health team don’t acknowledge their individual implicit biases, we will still leave a large hole in the potential to address bias in healthcare. The entire interprofessional team, including clinicians, nurses, pharmacists, therapists, and other ancillary and administrative personnel, is responsible for openly discussing implicit biases influencing the care provided and keeping one another accountable.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Harini Shah declares no relevant financial relationships with ineligible companies.
Disclosure: Julie Bohlen declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Shah HS, Bohlen J. Implicit Bias. [Updated 2023 Mar 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- A Shadow of Doubt: Is There Implicit Bias Among Orthopaedic Surgery Faculty and Residents Regarding Race and Gender? [Clin Orthop Relat Res. 2024] A Shadow of Doubt: Is There Implicit Bias Among Orthopaedic Surgery Faculty and Residents Regarding Race and Gender? Gilbert SR, Torrez T, Jardaly AH, Templeton KJ, Ode GE, Coe K, Patt JC, Schenker ML, McGwin G, Ponce BA, et al. Clin Orthop Relat Res. 2024 Jul 1; 482(7):1145-1155. Epub 2024 Jan 12.
- Review Evidence Brief: The Quality of Care Provided by Advanced Practice Nurses [ 2014] Review Evidence Brief: The Quality of Care Provided by Advanced Practice Nurses McCleery E, Christensen V, Peterson K, Humphrey L, Helfand M. 2014 Sep
- The effectiveness of mindfulness based programs in reducing stress experienced by nurses in adult hospital settings: a systematic review of quantitative evidence protocol. [JBI Database System Rev Implem...] The effectiveness of mindfulness based programs in reducing stress experienced by nurses in adult hospital settings: a systematic review of quantitative evidence protocol. Botha E, Gwin T, Purpora C. JBI Database System Rev Implement Rep. 2015 Oct; 13(10):21-9.
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. [Cochrane Database Syst Rev. 2022] Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, et al. Cochrane Database Syst Rev. 2022 Feb 1; 2(2022). Epub 2022 Feb 1.
- Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics [ 2014] Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics Peterson K, McCleery E. 2014 May
Recent Activity
- Implicit Bias - StatPearls Implicit Bias - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Product overview
- All features
- Latest feature release
- App integrations
- project icon Project management
- Project views
- Custom fields
- Status updates
- goal icon Goals and reporting
- Reporting dashboards
- asana-intelligence icon Asana AI
- workflow icon Workflows and automation
- portfolio icon Resource management
- Capacity planning
- Time tracking
- my-task icon Admin and security
- Admin console
- Permissions
- list icon Personal
- premium icon Starter
- briefcase icon Advanced
- Goal management
- Organizational planning
- Project intake
- Resource planning
- Product launches
- View all uses arrow-right icon
- Work management resources Discover best practices, watch webinars, get insights
- Customer stories See how the world's best organizations drive work innovation with Asana
- Help Center Get lots of tips, tricks, and advice to get the most from Asana
- Asana Academy Sign up for interactive courses and webinars to learn Asana
- Developers Learn more about building apps on the Asana platform
- Community programs Connect with and learn from Asana customers around the world
- Events Find out about upcoming events near you
- Partners Learn more about our partner programs
- Asana for nonprofits Get more information on our nonprofit discount program, and apply.
- Project plans
- Team goals & objectives
- Team continuity
- Meeting agenda
- View all templates arrow-right icon
- Leadership |
- 19 unconscious biases to overcome and h ...
19 unconscious biases to overcome and help promote inclusivity
Unconscious biases are learned assumptions, beliefs, or attitudes that we aren’t necessarily aware of. While bias is a normal part of human brain function, it can often reinforce stereotypes. To combat unconscious bias, learn about different types of biases, how they might surface at work, and how to avoid them so you can build a more inclusive and diverse workplace.
That being said, these biases can lead to skewed judgments and reinforce stereotypes, doing more harm than good for companies when it comes to recruitment and decision-making.
It’s especially important to be aware of these biases during the hiring process since they can impact the success of your future team.
To help you recognize and combat unconscious bias in the workplace, we cover 19 unconscious bias examples and prevention strategies. Taking the steps to reduce biases will help you improve inclusivity, trust, and productivity within your company.
What is unconscious bias?
Unconscious bias, also known as implicit bias, is a learned assumption, belief, or attitude that exists in the subconscious. Everyone has these biases and uses them as mental shortcuts for faster information-processing.
Implicit biases are developed over time as we accumulate life experiences and get exposed to different stereotypes.
According to the Kirwan Institute for the Study of Race and Ethnicity , “These biases, which encompass both favorable and unfavorable assessments, are activated involuntarily and without an individual’s awareness or intentional control.”
As a result, unconscious biases can have a big influence on our limiting beliefs and behaviors. When this translates to our professional lives, it can affect the way we hire, interact with colleagues, and make business decisions.
If not properly addressed, these biases can negatively impact a company’s workplace culture and team dynamics.
Although these biases are pervasive, you can reduce their impact with deliberate attention and effort. Being aware of and understanding the different types of biases that exist can help you find ways to combat them.
Leading through change: Creating clarity and building trust
In this webinar, Asana experts outline concrete tips to guide your team through uncertainty. Learn how to help employees focus on what matters.
Types of unconscious bias
Unconscious biases manifest in different ways and have varying consequences. Some biases arise from judging people’s appearances, some are derived from preconceived notions, and others are borne of logical fallacies. We explore these common biases in detail below.
1. Gender bias
Gender bias, the favoring of one gender over another, is also often referred to as sexism. This bias occurs when someone unconsciously associates certain stereotypes with different genders.
This type of bias may affect recruitment practices and relationship dynamics within the company. An example of this bias during hiring is if the hiring panel favors male candidates over female candidates even though they have similar skills and job experience.
Another well-known example is the gender pay gap. As of 2021, the average median salary for men is about 18% higher than women’s.
The gender bias may reduce job and career advancement opportunities for certain populations.
How to avoid gender bias
Here are some ways to create a more gender-diverse workplace:
Set gender-neutral recruitment standards: Define the ideal candidate profile ahead of time and evaluate all candidates against those standards.
Create diversity goals: Set qualitative gender diversity goals to create a more gender-balanced team. Support and provide resources for women to take on leadership roles.
Ageism refers to stereotyping or discriminating against others based on their age, often happening to older team members.
Although workers ages 40 and older are protected from workplace discrimination under the Age Discrimination in Employment Act, filing for a lawsuit against an employer can be a lengthy and costly process.
Because not everyone files a complaint, ageism is still a prevalent issue. An AARP survey found that about 60% of workers age 45 and older have seen or experienced age discrimination in the workplace.
An example of ageism is if an older team member was passed over for a promotion, which ended up going to a younger team member with less seniority and experience.
Companies that discriminate based on age may lose out on the valuable knowledge and experience that older workers bring. There may also be serious legal consequences if a team member decides to file a job discrimination lawsuit.
How to avoid ageism bias
Preventing ageism involves combatting age-related stereotypes as well as engaging older team members in the workplace. Here are some ways to do that:
Don’t make assumptions based on age: For example, don’t automatically presume that older workers don’t know how to use technology or aren’t open to learning new skills. Provide equal learning opportunities for everyone.
Foster cross-generational collaboration: Create two-way mentorship programs where a senior team member is paired with a new hire. This kind of collaboration facilitates communication between team members of different stages, which can help break down misconceptions about age.
3. Name bias
Name bias is the tendency to prefer certain names over others, usually Anglo-sounding names.
Name bias is most prevalent in recruitment. If a recruiter tends to offer interviews to candidates with Anglo-sounding names over equally qualified candidates with non-Anglo names, this bias is present.
Name bias can have a negative impact on diversity hiring and result in companies missing out on talented candidates.
How to avoid name bias
A simple solution to avoid name bias is to omit names of candidates when screening. To do this, you can:
Use software: Use blind hiring software to block out candidates’ personal details on resumes.
Do it manually: Designate a team member to remove personal information on resumes for the hiring team.
4. Beauty bias
Beauty bias refers to the favorable treatment and positive stereotyping of individuals who are considered more attractive. This has also given rise to the term “ lookism ,” which is discrimination based on physical appearance.
An example of beauty bias is a hiring manager who is more inclined to hire candidates they think are good-looking.
Hiring decisions should be based on skills, experience, and culture fit rather than physical appearance.
How to avoid beauty bias
Here are some ways to avoid beauty bias when screening job applicants:
Omit pictures from resumes: Focus on an applicant’s qualifications and experience when screening resumes.
Conduct telephone screening: Before scheduling an interview, consider doing a short telephone interview to get to know the applicant better without being influenced by their appearance.
5. Halo effect
The halo effect, a term coined by psychologist Edward Thorndike in the 1920s, occurs when we develop an overall positive impression of someone because of one of their qualities or traits.
This effect may lead us to inadvertently put people on a pedestal since we’re constructing an image of a person based on limited information.
An example of this effect in recruitment is when a hiring manager sees that a candidate graduated from a prestigious school and assumes that they excel at their job.
This halo is based on the hiring manager’s academic preferences. However, the school that someone went to doesn’t necessarily determine their level of job competency.
By focusing too much on one positive trait, we may overlook negative behavior that could end up harming the company—for example, if a candidate was fired for misconduct in a previous job.
How to avoid the halo effect
To reduce the impact of the halo effect, you could try out different interviewing strategies:
Conduct multiple interviews: Set up several rounds of interviews for candidates with different levels of management. That way, a candidate can be evaluated from various perspectives.
Diversify your interview team: Getting someone from another team to interview the candidate may help since they’ll have less reason to “halo” them as they won’t be working with them directly.
6. Horns effect
The horns effect is the opposite of the halo effect. This bias causes us to have a negative impression of someone based on one trait or experience.
Putting too much weight on a single trait or interaction with someone can lead to inaccurate and unfair judgments of their character.
For example, a new team member thinks the constructive criticism they received from their manager is harsh and assumes that their manager is a critical and stern person.
If left unchecked, the horns effect can damage the cohesiveness and trust between team members.
How to avoid the horns effect
In order to reduce the horns effect when interacting with others, try to:
Challenge your first impressions: Take the time to get to know someone so you can develop a more concrete impression of that person as a whole.
Make judgments based on evidence: Ask yourself how you developed your first impression of someone and find evidence to support or refute that impression based on additional interactions.
7. Confirmation bias

Confirmation bias is the tendency to seek out and use information that confirms one’s views and expectations. In other words, cherry-picking information to validate certain points.
This affects our ability to think critically and objectively, which can lead to skewed interpretations of information and overlooking information with opposing views.
For example, a product developer comes up with a product idea for the athletic market. Although market research shows little interest in the product, they try to validate the idea by reaching out to athlete friends who they know will support the idea.
Although there’s gratification in validating a current idea, it’s important to consider the potential consequences of following through with the idea.
How to avoid confirmation bias
Here are some ways to reduce confirmation bias:
Gather multiple sources: Whenever you’re testing a hypothesis or conducting research, gather information from a wide variety of sources to get a balanced perspective.
Standardize interview questions : When recruiting new talent, come up with a list of standard interview questions to prevent asking off-topic or pointed questions that may or may not confirm your beliefs about a candidate.
8. Conformity bias
Conformity bias is similar to groupthink, which occurs when we change our opinions or behaviors to match that of the bigger group, even if it doesn’t reflect our own opinions.
This bias may occur when we encounter peer pressure or are trying to fit into a certain social group or professional environment.
For example, a team is deciding between two proposals. One person thinks proposal A is better, but the rest of the team is leaning towards proposal B. That person is swayed by their opinions and ends up voting for proposal B because everyone else did.
Although conformity can help prevent conflicts, it may also limit creativity, open discussions, and having other perspectives available.
How to avoid conformity bias
Here are some ways to help encourage honest opinions in the workplace:
Use anonymous votes or surveys: The option to give feedback anonymously allows the freedom to express opinions without worrying about others’ preferences.
Ask for opinions in advance: Before going into a meeting, have a private conversation with each team member to get their opinions. This gives everyone plenty of time to think about a topic and express their thoughts without the pressure of presenting in front of colleagues.
9. Affinity bias
Affinity bias is also known as the similarity bias and refers to the tendency to favor people who share similar interests, backgrounds, and experiences. We tend to feel more comfortable around people who are like us.
This bias may affect hiring decisions. For example, a hiring manager gravitates towards a job applicant because they share the same alma mater.
Over time, the affinity bias in hiring can hamper a company’s diversity and inclusion efforts.
How to avoid affinity bias
While eliminating affinity bias entirely may not be possible, there are ways to reduce its effects:
Create a diverse hiring panel: Different people with varying perspectives and interests that conduct interviews can help reduce the affinity bias of one individual.
Go beyond hiring for “culture fit": The more hiring managers have in common with candidates, the more likely they are to evaluate them as a good “culture fit.” But the term "culture fit" is vague, and it can mean different things to different people. To assess candidates fairly, use specific language and examples when sharing feedback about them. Describe how well they embody company values or align with company missions.
10. Contrast effect
We often make judgments by making comparisons. As a result, our judgments may be altered depending on what standard we’re comparing something to. This is known as the contrast effect.
For instance, a team member is happy to receive a “meets expectations” on their performance review. However, they start to feel inadequate after finding out most of their colleagues got “exceeds expectations” on their reviews.
Even though they got a decent review, the team member judges themselves more critically since their comparison standard is their colleagues’ results.
There can also be positive contrast effects, which occur when something is perceived to be better than usual because it’s being compared to something worse.
How to avoid the contrast effect
Here are some strategies to try when using comparisons to make decisions:
Make multiple comparisons: Instead of coming to a conclusion after making one comparison, compare something against different standards to broaden your perspective.
Talk it out: Explain how you came to a given conclusion to your colleagues so they can understand your point of view.
11. Status quo bias
This bias describes our preference for the way things are or for things to remain as they are, which can result in resistance to change.
Following the status quo is a safe option and takes less effort, but it also results in becoming stagnant. As the business landscape continues to shift, change is necessary for business longevity and innovation.
An example of the status quo bias in a company is continuing to hire team members from the same demographic group, making no effort to move forward with diversity goals.
By repeatedly engaging in the same hiring practices, you may miss out on great candidates who can bring fresh ideas and perspectives to your company.
How to avoid the status quo bias
Here are some ways you can challenge the status quo:
Use the framing effect: We often follow the status quo to avoid a loss, which we place greater weight on compared to gains. The framing effect involves looking at the default option as a loss to encourage exploring alternative options as gains.
Encourage outside-the-box thinking: Create an environment that celebrates creativity and innovation. Adapt an open mindset to change so that your team can continue to push the status quo.
12. Anchor bias
Anchor bias occurs when we overly rely on the first piece of information we receive as an anchor to base our decision-making upon. This causes us to see things from a narrow perspective.
For example, the first thing a recruiter finds out about a candidate they’re interviewing is that they were unemployed for the past year. The recruiter focuses on this fact rather than the candidate’s solid qualifications and skills.
Instead of relying on one piece of information to make a decision, it’s important to look at the whole picture.
How to avoid anchor bias
It takes time to make a thoughtful decision. Here are some tips to keep in mind:
Conduct thorough research: The first option may not always be the best one. Explore various possible options and their pros and cons before deciding.
Brainstorm with your team: Discussing a given decision with your teammates can help reveal the strengths and weaknesses of a plan.
13. Authority bias

Authority bias refers to the tendency to believe in authority figures and follow their instructions.
Generally, following a trusted authority figure with relevant expertise is a good idea. However, blindly following a leader’s direction without your own critical thinking may cause future issues.
For example, if a team member unquestionably follows their manager’s instructions to write a report in a way that matches the manager’s opinions, this could jeopardize the integrity of the report.
When receiving instructions on an area outside of your manager’s expertise, it can be worthwhile to seek additional information or expertise to minimize potential issues that may arise.
How to avoid authority bias
As with many unconscious biases, developing awareness of the bias is a good first step to countering it.
Here is how to avoid being influenced by authority bias:
Ask questions: Don’t be afraid to ask your manager or company leader questions. The level of detail they provide may be an indicator of whether an idea was well thought-out or if it’s their authority coming into play.
Do your research: Conduct your own research on a given topic to identify other credible sources or experts and see whether their suggestions align with your manager’s suggestions.
14. Overconfidence bias
Overconfidence bias is the tendency for people to think they are better at certain abilities and skills than they actually are.
This false assessment of our skill levels, stemming from an illusion of knowledge or control, can lead us to make rash decisions.
For instance, an overconfident CEO decides to acquire a startup that they see high potential in and believe will bring high returns even though their performance indicates otherwise.
Previous success or accomplishments may lead to an inflated ego. While leading with confidence is a good thing, it’s important to not let it get in the way of logical thinking and decision-making.
How to avoid overconfidence bias
Here are tips to follow when you’re making decisions:
Consider the consequences: The decisions you make can have an impact on your company. Before committing to a decision, determine all the possible outcomes to ensure you’re prepared for them.
Ask for feedback: Getting feedback from your team can help you identify areas of improvement, whether it’s related to your performance or your ideas. Constructive criticism can keep egos in check.
15. Perception bias
Perception bias occurs when we judge or treat others based on often inaccurate, overly simplistic stereotypes and assumptions about the group they belong in. It may involve other biases such as gender, age, and appearance.
This type of bias may result in social exclusion, discrimination, and an overall reduction of a company’s diversity goals.
Say, for example, a team member doesn’t invite a teammate to an after-work social event because they assumed that they wouldn’t share similar interests with the group.
Perception bias can make it difficult to have an objective understanding about members from diverse groups.
How to avoid perception bias
Reducing the impact of perception bias requires recognizing your biases:
Challenge your assumptions: Ask yourself, “How well do I really know that person or the group they belong to?” Don’t let preconceived notions prevent you from meeting or including new people.
Think about the accuracy of statements: When you find yourself using strong words like “all,” “always,” and “never” to describe a certain group, pause and take a moment to ask yourself how accurate the description is.
16. Illusory correlation
Illusory correlation is when we associate two variables, events, or actions together even though they’re unrelated to each other.
For example, a hiring manager asks a candidate interview questions in an effort to gain insight into their personality but are unrelated to the job itself. Since the candidate struggles to come up with answers, the hiring manager decides they would not be a good fit.
These illusions can leads us to making decisions based on inaccurate correlations.
How to avoid illusory correlation bias
We may be more prone to see false correlations in circumstances that we’re unfamiliar with or have little knowledge of.
Here are tips to avoid making illusory correlations:
Get informed: Learning more about the areas you’re not familiar with can help you find evidence to support or refute the correlation.
Consider all possibilities: When you associate two things, consider the likelihood of the cause and effect. You can also use a contingency table to visualize the relationships between the cause and effect.
17. Affect heuristic
Heuristics are mental shortcuts that help us make decisions more efficiently. The affect heuristic occurs when we rely on our emotions to make decisions. This may help us reach a conclusion more quickly, though it may not always be accurate or fair.
For example, an interview candidate makes an off-hand comment that offends a recruiter, though that wasn’t their intention. The recruiter decides to reject the candidate because they were vexed by the comment even though they were the most qualified candidate.
Since emotions may cloud your judgment, it’s important not to make decisions in the heat of a moment.
How to avoid the affect heuristic bias
Here are ways to lower the influence of emotions in different circumstances:
Be aware of your emotions: Simply being aware of our level of emotions in a situation can help us step back from the situation and evaluate it more logically.
Take time to reflect: Reflect on an event some time after it occurs. Your emotions likely won’t be as strong as they were during the event, so you’ll be able to come to a more objective conclusion.
18. Recency bias
Recency bias occurs when we attribute greater importance to recent events over past events because they’re easier to remember.
This bias is more likely to occur when we have to process a large amount of information. For example, since hiring managers often review a high volume of job applications in a day, it may be harder to recall candidates screened earlier during the day.
Recency bias can also manifest during the interview process when a hiring manager becomes more inclined to make hiring decisions based on the most recent candidate they interviewed.
To overcome this bias, using techniques to strengthen your memory can be helpful.
How to avoid recency bias
Here are some tips to prevent recency bias when interviewing candidates:
Take notes: Take detailed notes during each interview and review them afterward. This can help you keep track of notable candidates regardless of when you interviewed them.
Give yourself mental breaks: Doing back-to-back interviews can be mentally draining. When your working memory takes a toll, you’re more likely to be affected by recency bias. Stay mentally alert by taking breaks in between interviews so your brain has time to absorb and remember the information.
19. Idiosyncratic rater bias
Idiosyncratic rater bias affects the way we evaluate the performance of others. We often rate others based on our subjective interpretations of the assessment criteria and our own definition of what “success” looks like.
In other words, we’re generally unreliable when it comes to rating other people. Research has found that about 60% of a manager’s rating is a reflection of the manager rather than the team member they’re rating.
For example, a manager who excels at project management has higher standards for this skill and gives harsher ratings to team members for this skill. On the other hand, the manager is more lenient when rating team members’ marketing skills because they are less familiar with that area.
Sources of rater bias may come from other biases, such as the halo effect, affinity bias, and confirmation bias.
How to avoid idiosyncratic rater bias
Here are some strategies to avoid this bias when doing performance reviews:
Set specific and clear assessment criteria: Create a rubric or a specific set of standards for evaluating performance. This prompts managers to provide supporting evidence based on a team member’s performance or achievements to determine how well they did.
Conduct multi-rater reviews: This process involves a team member getting feedback from their colleagues and managers in addition to doing a self-evaluation. Having multiple reviews to draw from can help managers gain a more holistic view of a team member’s performance and identify potential areas for growth.
Why it’s important to tackle unconscious biases
As these examples show, unconscious biases can hinder decision-making, impact team dynamics and leadership styles , and limit company diversity. This, in turn, can reduce equal opportunities for team members and job applicants.
Tackling unconscious biases can help address these issues, as well as improve company diversity.
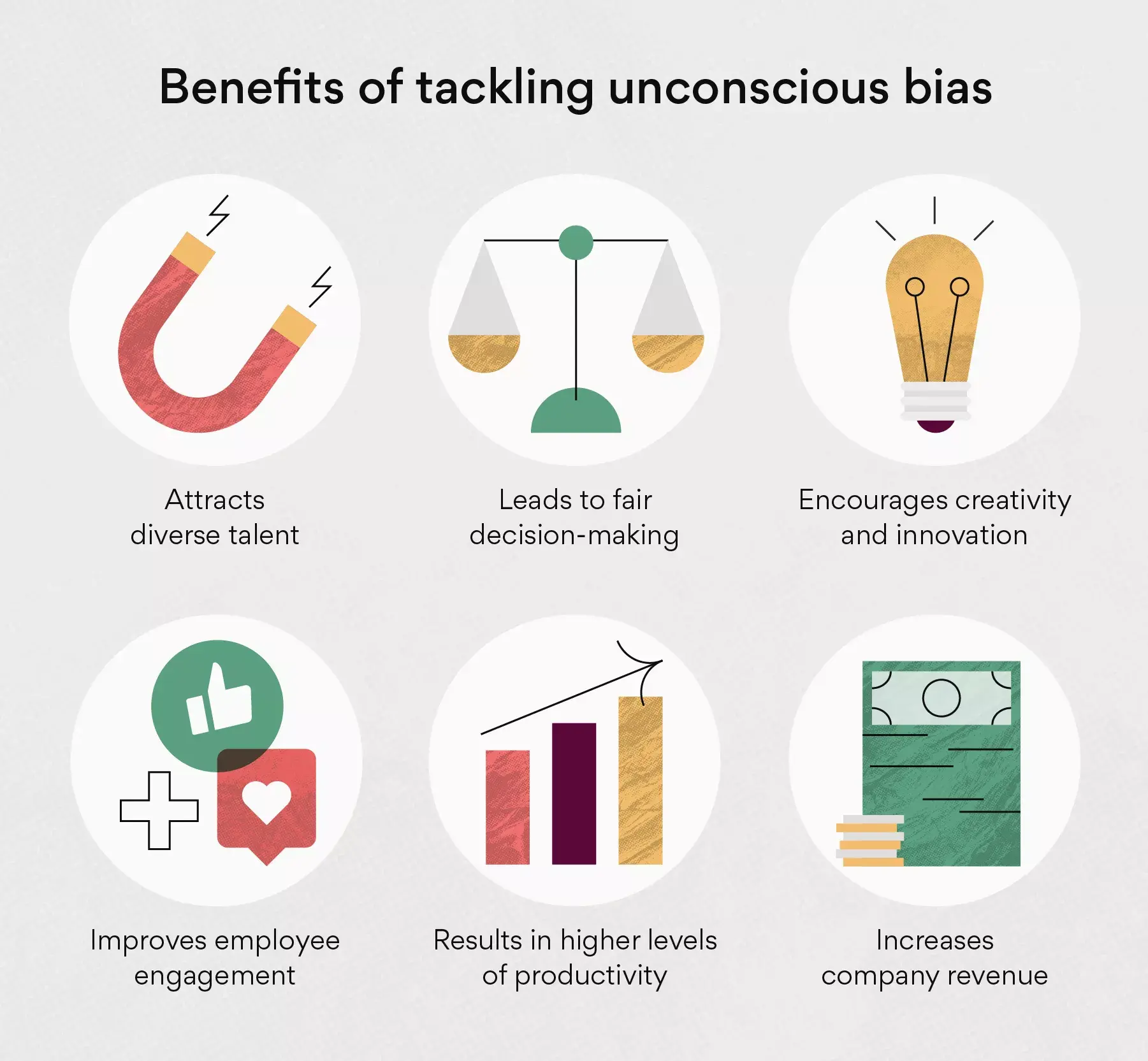
Increased company diversity can bring additional benefits such as:
Increasing company profitability: Teams that have solid problem-solving and decision-making skills can bring a competitive advantage to a company. For example, a McKinsey study found that gender-diverse companies were 21% more likely to gain above-average profitability.
Attracting diverse talent through inclusive hiring practices: By implementing inclusive recruitment strategies, companies are able to reach out to a wider talent pool. Job seekers would also be more likely to apply to companies that prioritize diversity.
Increasing innovation: Diverse teams can bring a variety of fresh ideas to the table, allowing teams to come up with creative solutions that can drive sales. For example, a study by the Boston Consulting Group found that companies with diverse management teams bring 19% higher innovation revenue.
Boosting company productivity: University research found that tech firms with diverse management teams have 1.32 times higher levels of productivity . Increased productivity can lead to more efficient project management and implementation.
Encouraging higher employee engagement: Deloitte research showed that company diversity is directly related to employee engagement . Higher employee engagement can lead to higher job satisfaction, which in turn, can lower the turnover rate.
Making fair and more efficient business decisions: Inclusive teams can make better business decisions up to 87% of the time. These business decisions can help improve a company’s performance and revenue.
Be conscious of your unconscious biases
The good news: Once you’re aware of your unconscious biases, you can take steps to mitigate their effects. By taking micro-steps such as revamping your interview questions template and encouraging cross-team collaboration , you’re working towards a more diverse and inclusive workplace environment for you and your team.
Related resources

How to give and take constructive criticism
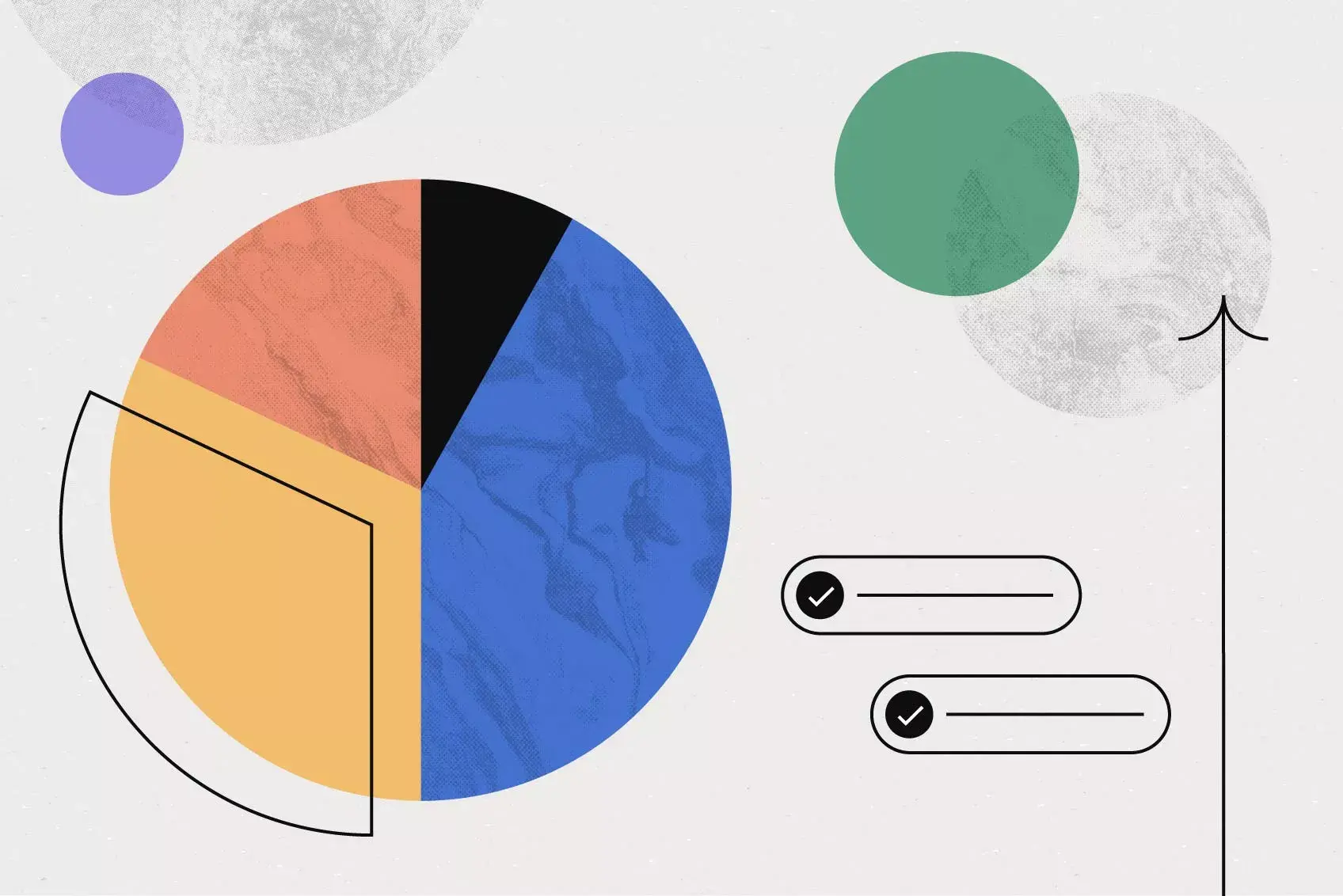
Data-driven decision making: A step-by-step guide

Listening to understand: How to practice active listening (with examples)

How executives and individual contributors differ when it comes to AI
11 Examples of Unconscious Bias in the Workplace
- September 11, 2024

Share This Article
- Unconscious bias may lead to unfair treatment. This may particularly apply in the workplace because of predetermined beliefs about a person’s identity.
- Several unconscious biases can affect employees and leadership in workplace organizations. This includes name bias, racial bias, gender bias and anchoring bias.
- Unconscious bias in the workplace can be solved through different tactics. These may include diverse hiring panels and education and training programs.
Table of Contents
Unconscious bias plays a big role in workplaces around the globe, where individuals of different backgrounds come together. Many people have good intentions. However, some may unknowingly let preconceived notions or experiences influence their judgment of others. This can impact decisions made by recruiters or interactions between colleagues. Unconscious bias can lead to unfair treatment or missed opportunities for those who are judged.
Ahead, we discuss what unconscious bias is and why it is important to address it. We will also cover examples of unconscious bias in the workplace and the effects of unconscious bias on organizations.
What Is Unconscious Bias?
Unconscious bias is the quick and unintentional judgments people form about others based on their background, appearance or other characteristics. Unconscious bias is also referred to as implicit bias .
These biases can be formed through exposure to false information and stereotypes. They may also be influenced by other factors, including the media, family systems or a lack of exposure to diversity. Unconscious biases occur in everyday life, including in workplace culture.
Why Is It Important to Address Unconscious Bias at Work?
It is critical to address unconscious bias because it is essential for creating a fair, inclusive and productive workplace. It also reduces discrimination and fosters a culture of inclusivity. Addressing unconscious bias can lead to better mental health for employees, higher job satisfaction and lower employee turnover. It may also lead to improved market success, increased employee engagement and more innovative and diverse perspectives. Biases can be reduced through dedicated conversations, training and equitable hiring practices.
11 Examples of How Unconscious Bias Affects the Workplace
Unconscious bias can manifest in different ways. Take a look below at 11 types of unconscious bias that can affect the workplace.
1. Confirmation Bias
Confirmation bias (or cognitive bias) leads people to search for data and information that aligns with their beliefs. These individuals may become siloed in their belief systems. They may not extend their knowledge beyond what they know or seek other information that may dispute it. Understanding this bias and tackling it can lead to a more well-rounded viewpoint and mindset.
In the workplace, this bias may result in individuals not accepting others’ points of view or not expanding their own. This can lead to less collaboration and reasonable decision-making among team members. It can also impact candidates in the hiring process.
2. Racial Bias
Racial bias is a type of unconscious bias. That is because people may subconsciously base their thoughts and actions on assumptions about someone’s race.
A Pew Research Center survey from 2022 reported that racial and ethnic bias is an issue in workplace practices. According to the survey, 64% of Black American adults said it is a major problem in hiring, compared to 30% of their white counterparts. In addition, 56% of Black Americans said racial and ethnic bias was an issue in performance reviews, compared to 23% of their white counterparts.
Racial bias in the workplace can affect an individual’s sense of belonging and create teams that lack diversity and inclusiveness. Ultimately, it can impact how employees feel about their career path and future with an organization.
Some organizations have started using artificial intelligence (AI) during hiring and performance evaluations to reduce this bias. Based on the survey mentioned above, many think that AI could help create more fair and equitable outcomes by minimizing the influence of racial bias.
3. Gender Bias
Gender bias is a type of unconscious bias where a person favors one gender identity over another. Or they attach particular stereotypes to different gender expressions. In the workplace, this bias can lead to inequalities in performance rewards, support or mentorship opportunities. It can also appear in compensation and exacerbate the gender pay gap.
According to the 2022 Deloitte Women @ Work report, 59% of women stated they had experienced microaggressions and other mistreatment in the workplace. This percentage increased from the year prior, a reported 52%. According to the data, more than 90% of women feel that disclosing this type of mistreatment will result in harmful consequences to their careers.
4. Attribution Bias
Attribution bias occurs when a person judges another person’s actions based on previous interactions or information. This can lead to assumptions and inaccurate conclusions about them. This commonly happens without considering the full context of their background or personality. In the workplace, it is important to get a comprehensive understanding of an individual’s situation before forming an opinion.
5. Affinity Bias
People hold affinity bias (or similarity bias) when they favor individuals who share similar interests, backgrounds and experiences. In an organization, affinity bias may occur when searching for candidates from particular companies or educational institutions. This form of bias can lead to unequal opportunities and hinder diversity and inclusion.
6. Conformity Bias
Conformity bias, also known as groupthink, occurs when individuals adopt the views or opinions of the majority instead of thinking independently. This type of unconscious bias can impact creativity, as people may prioritize consensus over innovative solutions. In the workplace, conformity bias can appear during meetings or during board votes, where the pressure to align with the group can impact decisions.
7. Affect Heuristic
Affect heuristic means we depend on our emotions rather than facts to make decisions. This form of bias can lead to irrational or unfair choices. For example, someone may favor a project because it “gives them a good feeling” rather than using solid evidence. In a workplace, affect heuristic can negatively impact decision-making and lead to less effective results.
8. Contrast Effect
Contrast effect is the comparison of multiple subjects or individuals. In the workplace, this could refer to comparing candidates or employees who are up for a job or promotion. Equally comparing candidates in the interview process and employees for role advancement may combat the contrast effect and mitigate bias in organizations. This type of unconscious bias can create a negative workplace culture and culminate in lower diversity rates and employees leaving a company.
9. Beauty Bias
Beauty bias, or attractiveness bias, is when people are presumed to be more qualified and accomplished based on their physical appearance. In the workplace, this can lead to favored or unfair treatment of employees based on their appearance. Holding this type of bias can eventually result in higher turnover in the organization.
One way to prevent beauty bias is to perform phone screenings before a video or in-person interview to get to know potential hires. Another way is to exclude photos from candidates’ resumes.
10. Name Bias
Name bias is a type of unconscious bias where someone makes assumptions about an individual based on their first and last name. A Harris Poll survey reported the beliefs of over 2,000 U.S. employees regarding names. About 36% of persons of color surveyed said their name typically gets mispronounced, compared to 18% of their white counterparts. Approximately 33% of the people of color surveyed said they came in contact with discrimination at the workplace because of their names. This was in comparison to 16% of their white counterparts.
In the workplace, this type of bias and the mispronunciation of names can cause individuals to avoid communication or collaboration with other team members and can lower employee morale.
11. Anchoring Bias
Anchoring bias can cause individuals to make decisions solely based on initial information received. A person may make all future decisions based on that initial information. In the workplace, anchoring bias can present as individuals not embracing new ideas from their teammates or not asking for a second opinion on a client matter. Seeking other resources in the workplace may help mitigate inaccurate decision-making. It can also help eliminate anchoring bias.
The Effects of Unconscious Bias in the Workplace
From initial resume screenings to performance assessments, unconscious bias can negatively affect the workplace. It can also hinder efforts to diversify an organization.
How to Overcome Unconscious Bias
Fortunately, unconscious bias can be resolved through many factors, including enforced company policies and using inclusive language in company communications. In addition, building a diverse workforce, using multifaceted hiring panels and holding routine education sessions can help eradicate unconscious bias.
Stay up to date with the latest from Robert F. Smith about the importance of addressing unconscious bias in the workplace by following him on LinkedIn .
Aspire to be someone who inspires?
Learn how to become a better leader from philanthropist Smith.
Follow Robert F. Smith on social media for the latest on his work as a business and philanthropic leader.
Priority Initiatives
Privacy Policy

Across our Communities
Mbe entrepreneurship & supplier diversity.
1. Provide technical expertise: offer subject matter and technical expertise to catalyze and support community initiatives
E.g., tax/accounting experts to help MBEs file taxes
E.g., business experts to help MBEs better access capital and craft business plans to scale their teams and operations
Access to Capital (CDFI/MDI)
2. Fund modernization & capacity-building and provide in-kind subject matter experts – $30M: help 4-5 CDFIs/MDIs over 5 years modernize their core systems, hire and train staff, expand marketing and standup SWAT team of experts to conduct needs diagnostic, implement tech solution & provide technical assistance
Systems and technology modernization – $10M-15M: Add/upgrade core banking systems, hardware and productivity tools, train frontline workforce on new systems & technology and hire engineering specialists to support customization and news systems rollout – over 5 years
Talent and workforce – $10M: hire and train additional frontline lending staff and invest in recruiting, training, compensation & benefits and retention to increase in-house expertise and loan capacity – over 5 years
Other capacity-building and outreach – $8M: hire additional staff to increase custom borrower and technical assistance (e.g., credit building, MBE financing options, etc.) and increase community outreach to drive regional awareness and new pipeline projects – over 5 years
Education/HBCU & Workforce Development
3. Offer more paid internships: signup onto InternX and offer 25+ additional paid internships per year to HBCU/Black students
Digital Access
4. Issue digital access equality bonds: issue equality progress bonds and invest proceeds into SCI’s digital access initiatives
5. Fund HBCU campus-wide internet – up to $50M in donations or in-kind: Partner with the Student Freedom Initiative to deliver campus-wide high-speed internet at ~10 HBCUs across SCI regions
6. Be an advocate for SCI priorities: engage federal and state agencies to drive policy and funding improvements to better support SCI’s near-term priorities
E.g., Engage the Small Business Administration and Minority Business Development Agency to increase technical assistance programs and annual spend to better support Minority Business Enterprises (MBEs) with capital and scaling needs
E.g., Ask the Federal Communications Commission (FCC) to include multi-dwelling unit connectivity in its new broadband connectivity maps and ask the National Telecommunications and Information Administration (NTIA) to allow non-FCC data in state broadband plans to unlock ~$285M in potential government broadband funding for 5 SCI regions
Directly Fund SCI
7. Invest directly into SCI (coming soon): provide funding for SCI to pool and invest in community initiatives that are most well-positioned for funding and can drive direct community impact.

Memphis, Tennessee
Lead community organization: The Collective Blueprint
Our ambition:
Increase the volume and value of Black-owned businesses – through corporate MBE spend and MBE startups & scaling
1. Scale technical assistance – $15M: fund* to expand technical assistance through business coaches and wrap-around services for 500+ MBEs over 5 years to help them scale from <$1M to $5M+ in annual revenue
2. Standup MBE fund – $15M: standup/scale MBE fund* to offer more flexible access to capital arrangements 400-500 MBEs over 5 years
* Lead organization: The Collective Blueprint ; Contributing local organizations for community strategy include (but not limited to): Community Unlimited , Women’s Business Center South , Epicenter , others
Estimated impact (of all initiatives): 2.3x increase in MBE value & 20K+ new jobs, boosting Black community’s net worth by ~$3B+
Modernize CDFI/MDI systems and tech as well as recruit and upskill talent to increase CDFI/MDI capacity and ability to inject more capital into Black communities
3. Provide loan guarantees – $15M: create a fund* to provide 80% loan guarantees over 5 years to encourage lender participation and inject more capital into the community
4. Conduct advocacy: ask US Treasury & Tennessee State to allow Tennessee CDFIs/MDIs to retain SSBCI capital & offer loan guarantees to boost loan issuance
5. Fund modernization & capacity-building and provide in-kind subject matter experts – $30M: help 4-5 CDFIs/MDIs** over 5 years modernize their core systems, hire and train staff, expand marketing and standup a SWAT team of experts to conduct needs diagnostic, implement tech solution & provide technical assistance
* Leading organizations for community strategy include (but not limited to): Community LIFT , Memphis CDFI Network , etc.
* In partnership with National Bankers Association and Appalachian Community Capital ; CDFIs/MDIs being considered include: Community Unlimited, Hope Credit Union, River City Capital, United Housing Inc, etc.
Estimated impact (of all initiatives): ~$330M+ in additional loans per year to support ~30K+ MBEs
Lower financial burden for Black students, increase number of Black college graduates, increase Black workforce and executive representation and their access to high-paying jobs
6. Standup training hub – $30M: fund* the establishment a world-class training hub that offers certificate-granting STEM and innovation programs in advanced manufacturing, health care, etc. to 10K+ youths
7. Fund SFI program – $7M: fund the Student Freedom Initiative’s Income Contingent Alternative to Parent Plus to support ~15 Black STEM students per year forever at 4 HBCUs**
* Lead organization: The Collective Blueprint ; Contributing local organizations for community strategy include (but not limited to): Greater Memphis Chamber and Workforce Midsouth
** Minority Serving Institutions / HBCUs with STEM programs being considered: Le Moyne-Owen, Baptist Memorial, University of Memphis, Rust College
Estimated impact (of all initiatives): 8K+ additional college graduates and 10K workers with high-paying wages to drive ~$1B+ in economic growth
Increase accessibility, affordability and adoption of high-speed Internet
8. Accelerate digital access initiatives – $75M: partner with local orgs* to invest in setting up internet connections / installing hotspots, offering laptops and supporting adoption (through government subsidy technical assistance and digital literacy) to connect ~135K homes to high-speed internet in the Memphis region
9. Raise community awareness & adoption of Emergency Broadband Benefit: increase door-to-door and community outreach in low-income neighborhoods to get households onto EBB to help connect ~135K unconnected households
* Lead organization: The Collective Blueprint ; Contributing local organizations for community strategy include (but not limited to): CodeCrew
Estimated impact (of all initiatives): ~135K households connected to high-speed internet to unlock ~$2B+ in economic potential

Houston, Texas
Lead community organization: Greater Houston Partnership
1. Scale team – ~$3M: hire 3-4 FTEs over 5 years for One Houston Together * to help companies increase MBE spend from ~2% to 5-10%+ as well as BIPOC workforce advancement and BIPOC board representation
2. Increase MBE certification and scale technical assistance – ~$2M: partner with One Houston Together * and the Houston Minority Supplier Development Council (HSMDC) ** to certify additional MBEs, develop Minority Business Finder database tool and provide resources and services to help local MBEs scale and participate in Pathways to Excellence program
3. Commit to increase racial diversity in supply chain and procurement: increase MBE spend in Greater Houston region* to 5-10%+
* One Houston Together serves as lead (please contact if you are interested in funding these initiatives)
** Houston Minority Supplier Development Council (HSMDC) serves as a partner organization (please contact if you are interested in learning more about this initiative)
Estimated impact (of all initiatives): 2.5x increase in MBE value & ~55K new jobs, boosting Black community’s net worth by ~$12B
4. Fund modernization & capacity-building and provide in-kind subject matter experts – $30M: help 4-5 CDFIs/MDIs* over 5 years modernize their core systems, hire and train staff, expand marketing and standup SWAT team of experts to conduct needs diagnostic, implement tech solution & provide technical assistance
* In partnership with National Bankers Association and Appalachian Community Capital ; CDFIs/MDIs being considered include: Unity National Bank, Unity Bank of Texas, PeopleFund, Houston Business Development Inc, etc.
Estimated impact (of all initiatives): ~$330M in additional loans per year to support ~30K MBEs
5. Fund SFI program – $120M: fund the Student Freedom Initiative’s Income Contingent Alternative to Parent Plus * to support ~1.2K Black STEM students per year forever at 7 HBCUs**
* Student Freedom Initiative serves as lead (main contact if you are interested in learning more and funding this initiative)
** Minority Serving Institutions / HBCUs with STEM programs being considered: Texas Southern University, University of Houston, Prairie View A&M University, Houston Baptist University, University of Houston-Clear Lake, University of Houston-Downtown, University of St Thomas.
Estimated impact (of all initiatives): 5K+ additional college grads & ~600 workers with senior exec positions / high-paying wages to drive ~$0.2B in economic growth
6. Accelerate SCI’s digital access initiatives – up to $80M in donations or in-kind: invest in setting up internet connections / hotspots, offer laptops/Chromebooks and support adoption (through government subsidy technical assistance and digital literacy) to connect ~145K homes to high-speed internet in the Houston region*
7. Raise community awareness & adoption of Emergency Broadband Benefit: increase door-to-door and community outreach in low-income neighborhoods to get households onto EBB to help connect ~145K unconnected households
* Community organization(s) being identified
Estimated impact (of all initiatives): ~145K households connected to high-speed internet to unlock ~$3B in economic potential

Greater New Orleans, Louisiana
Lead community organization: Urban League of Louisiana
1. Scale Black Business Works Fund – $10M: grow the Urban League of Louisiana’s Black Business Works Fund to support ~3K-4K MBEs over 5 years with emergency working capital needs to support/sustain ~$1B+ in annual revenues
2. Scale technical assistance – $20M: fund the Urban League of Louisiana , New Orleans Business Alliance , Thrive New Orleans and Propellor to scale bookkeeping, B2C payment, marketing support & subsidized rent to scale 200+ MBEs from <$1M to $5M+ in annual revenue
Estimated impact (of all initiatives): 2.5x increase in MBE value & 8K+ new jobs, boosting Black community’s net worth by ~$2B+
3. Fund modernization & capacity-building and provide in-kind subject matter experts – $30M: help 4-5 CDFIs/MDIs* over 5 years modernize their core systems, hire and train staff, expand marketing and standup SWAT teams to conduct needs diagnostic, implement tech solution & provide technical assistance
* In partnership with National Bankers Association and Appalachian Community Capital ; CDFIs/MDIs being considered include: New Orleans Business Alliance (community convener), Liberty, TruFund, LiftFund, NewCorp, etc.
4. Subsidize internships & apprenticeships – $40M: fund the New Orleans Youth Alliance , YouthForce NOLA and the Urban League of Louisiana to place and help subsidize apprenticeships, internships and other work-based learning experiences for ~20K young adults in high-pay sectors (e.g., energy)
5. Fund SFI program – $12M: fund the Student Freedom Initiative’s Income Contingent Alternative to Parent Plus to support ~120 Black STEM students per year forever at 3 HBCUs*
* Minority Serving Institutions / HBCUs being considered: Dillard University, Southern University – New Orleans and Xavier University of Louisiana
6. Scale career prep – ~$10M: scale the New Orleans Youth Alliance and YouthForce NOLA with 15-20 coaches over 5 years to equip ~20K young adults with skills for high-paying industries, job search & prep and subsidized transportation
Estimated impact (of all initiatives): ~2K additional college graduates and ~20K workers with high-paying wages to drive ~$1B in economic growth
7. Accelerate SCI’s digital access initiatives – up to $35M in donations or in-kind: partner with New Orleans’s Office of Information Technology & Innovation and Education SuperHighway to invest in setting up internet connections / hotspots, offering laptops/Chromebook and supporting adoption (through government subsidy technical assistance and digital literacy) to connect ~55K homes to high-speed internet in Greater New Orleans region
8. Raise community awareness & adoption of Emergency Broadband Benefit: increase door-to-door and community outreach in low-income neighborhoods to get households onto EBB to help connect ~55K unconnected households
Estimated impact (of all initiatives): 55K households connected to high-speed internet to unlock ~$1B in economic potential

Charlotte, North Carolina
Lead community organization: Charlotte Regional Business Alliance
1. Offer in-kind FTEs: provide 2-5 in-kind FTEs to the Charlotte Regional Business Alliance (CRBA) over 5 years to convene corporate partners, assess their MBE spend, develop pipeline to increase MBE spend to 5-10%+
2. Offer technical assistance expertise: partner with the Charlotte Regional Business Alliance (CRBA) to advise/mentor ~200 MBEs on capital/loan access to help them scale from <$10M to $50M+
3. Commit to supplier diversity: increase MBE spend in Charlotte region to 5-10%+
Estimated impact (of all initiatives): 3x increase in MBE value & ~13K new jobs, boosting Black community’s net worth by ~$2B+
4. Fund modernization & capacity-building and provide in-kind subject matter experts – $30M : help 4-5 CDFIs/MDIs* over 5 years modernize their core systems, hire and train staff, expand marketing and standup SWAT team of experts to conduct needs diagnostic, implement tech solution & provide technical assistance; in-kind experts to also help build out the MBE ecosystem through CDFIs/MDIs, market CDFI/MDI offerings and programs and help draft final loan agreements to qualify borrowers between investment fund(s) and CDFIs/MDIs
* CDFIs/MDIs being considered (examples and not exhaustive): Security Federal Bank, Institute / North Carolina Community Development Initiative, Sequoyah Fund Inc, Self-Help Credit Union, BEFCOR, Aspire Community Capital, etc.
* In partnership with National Bankers Association and Appalachian Community Capital ; CDFIs/MDIs being considered include: Security Federal Bank, Institute / North Carolina Community Development Initiative, Sequoyah Fund Inc, etc.
5. Fund SFI program – up to $10M: fund the Student Freedom Initiative’s HELPS program to support ~1.5K+ students per year at HBCUs* with emergency expenses – e.g., unexpected health costs, late rent payments, etc.
* Minority Serving Institutions / HBCUs in Charlotte that are being considered: Johnson C. Smith University, Johnson & Wales University – Charlotte, Charlotte Christian College
6. Provide in-kind staff: offer 2-5 FTEs to the Charlotte Regional Business Alliance (CRBA) over 5 years to track Black-/Brown-executive representation, convene corporate partners to develop executive pipeline and hiring plans and support corporate partners to increase representation from ~10% to 30%+
Estimated impact (of all initiatives): 2.5K+ additional college graduates and 2.5K workers with high-paying wages to drive ~$0.2B in economic growth
7. Raise community awareness & adoption of Emergency Broadband Benefit: increase door-to-door and community outreach in low-income neighborhoods to get households onto EBB to help connect ~35K unconnected households
Estimated impact (of all initiatives): ~35K households get connected to high-speed internet to unlock ~$700M in economic potential for Charlotte

Birmingham, Alabama
Lead community organization: Prosper Birmingham
1. Fund startups and give access to investor network – $70M: grow the Prosper Health Tech Fund – powered by Gener8tor – and offer venture capital technical assistance to scale 50+ startups from <$1M to $5M+ in annual revenue; near-term priority is to secure $4M in venture investment by end of May 2022
2. Fund technical assistance – $25M: fund Prosper Birmingham , Magic City Match , and Birmingham Business Alliance to establish/expand business advisory programs, renovate and subsidize retail/office space for MBEs and scale coaches & support services (e.g., digital footprint, B2C platforms, accounting & bookkeeping, recruitment, etc.) to help 100+ MBEs scale from <$1M to $5M+ in annual revenue
Estimated impact (of all initiatives): 3x increase in annual MBE revenue & 8K+ new jobs, boosting Black community’s net worth by ~$2B+
3. Fund modernization & capacity-building and provide in-kind subject matter experts – $30M: help 4-5 CDFIs/MDIs* over 5 years modernize their core systems, hire and train staff, expand marketing and standup SWAT team of experts to conduct needs diagnostic, implement tech solution & provide technical assistance
* In partnership with National Bankers Association and Appalachian Community Capital ; CDFIs/MDIs being considered include: First Bancshares, Commonwealth National Bank, TruFund, Sabre Finance, Bronze Valley, etc.
4. Fund scholarships and hire coaches – ~$35M: scale Birmingham Promise fund to financially support 200-250 students per year over 4 years to increase college retention and graduation rates
5. Fund endowment – $2M: support 50 University of Alabama at Birmingham college students per year with housing to reduce their financial burden and increase college retention and graduation rates
Estimated impact (of all initiatives): 6.5K+ additional college graduates & 35K workers with high-paying wages to drive ~$1.2B in economic growth
6. Raise community awareness & adoption of Emergency Broadband Benefit: increase door-to-door and community outreach in low-income neighborhoods to get households onto EBB to help connect ~35K unconnected households
Estimated impact (of all initiatives): 48K households get connected to high-speed internet to unlock ~$700M in economic potential for Jefferson County

IMAGES
VIDEO
COMMENTS
Introduction. Unconscious or implicit biases are attitudes or stereotypes that arise from preformed mental associations, which influence our understanding, actions, and decisions in an unconscious manner. 1 Unconscious biases are universal and have adverse consequences for the workplace, health care, and the learning environment. 2 - 4 Studies show that clinicians' negative implicit bias ...
The concept of implicit bias, also termed unconscious bias, and the related Implicit Association Test (IAT) rests on the belief that people act on the basis of internalised schemas of which they are unaware and thus can, and often do, engage in discriminatory behaviours without conscious intent.1 This idea increasingly features in public discourse and scholarly inquiry with regard to ...
Unconscious bias training has played a major role in their efforts. UB training seeks to raise awareness of the mental shortcuts that lead to snap judgments—often based on race and gender ...
Unconscious bias (also known as implicit bias) refers to unconscious forms of discrimination and stereotyping based on race, gender, sexuality, ethnicity, ability, age, and so on. It differs from ...
Unconscious bias refers to the automatic associations and reactions that arise when we encounter a person or group. Instead of maintaining neutrality, we tend to associate positive or negative stereotypes with certain groups and let these biases influence our behavior towards them. Example: Unconscious bias. An older woman is walking home from ...
What Science Has To Say About Unconscious Bias : Short Wave The human brain can process 11 million bits of information every second. But our conscious minds can handle only 40 to 50 bits of ...
DOI: 10.1056/NEJMp2201180. Implicit and explicit biases are among many factors that contribute to disparities in health and health care. 1 Explicit biases, the attitudes and assumptions that we ...
When Jennifer Eberhardt appeared on The Daily Show with Trevor Noah in April 2019, she had a hard time keeping a straight face. But some of the laughs were painful. Discussing unconscious racial bias, which she has studied for years, the Stanford University psychologist mentioned the "other-race effect," in which people have trouble recognizing faces of other racial groups.
2. Materials and Methods. We chose the method of a scoping review [] as our aim was to create an overview of the research conducted on unconscious bias during the last 10 years, to include a broad range of studies, to evaluate the scope of available research, and to identify research gaps [].In doing so, we followed the JBI International Scientific Committee's guide on conducting scoping ...
Banaji opened on Tuesday by recounting the "implicit association" experiments she had done at Yale and at Harvard. The assumptions underlying the research on implicit bias derive from well-established theories of learning and memory and the empirical results are derived from tasks that have their roots in experimental psychology and ...
Introduction Unconscious bias training: An assessment of the evidence for effectiveness by Doyin Atewologun, et al. is a literature review and meta-analysis of studies that examines the evidence for the effectiveness of unconscious bias training programs in actually reducing unconscious bias in individuals and organizations. The authors first define unconscious bias as the automatic and…
An earlier study of unconscious racial and social bias in medical students found unconscious white and upper-class preference on the IAT but no obvious unconscious preferences in students' response to vignette-based patient assessments . Unconscious bias affects the lived experiences of trainees, can potentially influence decisions to pursue ...
Research continues to reveal more about the nature and impacts of implicit bias — something hidden from our direct awareness that causes tangible damage in many spheres of life, even for the very young. ... Technology, and Law. The workshop engaged researchers and legal scholars in an exploration of implicit bias — unconscious favoritism ...
ous bias versus conscious biasIt is important to note that unconscious bias is not the same as having deliberate prejudices, which are referred to as 'conscious bi. s' or 'explicit bias ...
Biases are either conscious (explicit) or unconscious (implicit). Unconscious bias refers to personal biases that we are not aware of. It is the cause of our impulsive reactions of events that impact our lives resulting in quick judgements that may not be logical to others. Unconscious bias is the result of cognitive reasoning that was embedded ...
Unconscious biases are malleable-one can take steps to minimize the impact of unconscious bias (Dasgupta, 2013; Dasgupta & Greenwald, 2013). A substantial amount of research has been published demonstrating impact of unconscious bias in various domains including the criminal justice system, education, and health/health care (Kirwan Institute ...
This animation and briefing on unconscious bias adapted by Professor Uta Frith DBE FBA FMedSci FRS introduce the key concepts and current academic research around unconscious bias with the aim of alerting Royal Society selection and appointment panel members to potential biases that can arise when making judgments or decisions. They form part of the Society's efforts to ensure that all those ...
The Implicit Association Test (IAT) is the commonest measure of bias within research literature. It was developed from review work which identified that much of social behaviour was unconscious or implicit and may contribute to unintended discrimination. 16,17 The test involves users sorting words into groups as quickly and accurately as possible and comes in different categories from ...
Background: Unconscious biases are one of the causes of health disparities. Health professionals have prejudices against patients due to their race, gender, or other factors without their conscious knowledge. This review aimed to provide an overview of research on unconscious bias among health professionals and to investigate the biases that exist in different regions of the world, the health ...
by Michael Miller | Sep 4, 2018. A growing body of psychology research points to an uncomfortable truth about decision making: unconscious bias influences all of us and even the simplest decisions we make. Whether it's our level of hunger, the time of day, or our mood, there are quite a few internal and external factors that creep into our ...
UNCONSCIOUS BIAS IS HARD-WIRED. Deep within our subconscious, stereotypes are ingrained. Neuropsycholigists tell us cognitive bias is built into the very structure of the brain. Our unconscious brain processes and sifts vast amounts of information looking for patterns (200,000 times more than the conscious mind).
May 25, 2022. Unconscious Bias is an association or attitude about a person or social group that, while not plainly expressed, operates beyond our control and awareness, informs our perceptions, and can influence our decision-making and behavior. It exists in each person's worldview and affects our actions from the classroom to the workplace.
Combat unconscious bias in research with these strategies: peer review, blind procedures, and bias training for more precise analysis.
Implicit bias is the attitude or internalized stereotypes that unconsciously affect our perceptions, actions, and decisions. These unconscious biases often affect behavior that leads to unequal treatment of people based on race, ethnicity, gender identity, sexual orientation, age, disability, health status, and other characteristics. In ...
A simple solution to avoid name bias is to omit names of candidates when screening. To do this, you can: Use software: Use blind hiring software to block out candidates' personal details on resumes. Do it manually: Designate a team member to remove personal information on resumes for the hiring team. 4.
Unconscious bias is the quick and unintentional judgments people form about others based on their background, appearance or other characteristics. ... A Pew Research Center survey from 2022 reported that racial and ethnic bias is an issue in workplace practices. According to the survey, 64% of Black American adults said it is a major problem in ...
We've known for decades that unconscious biases shape our perceptions of men and women in the workplace. But what happens when we bring those biases to the voting booth during a presidential ...