Jump to navigation
- Bahasa Indonesia
- Bahasa Malaysia


Conclusions about the effects of electronic cigarettes remain the same

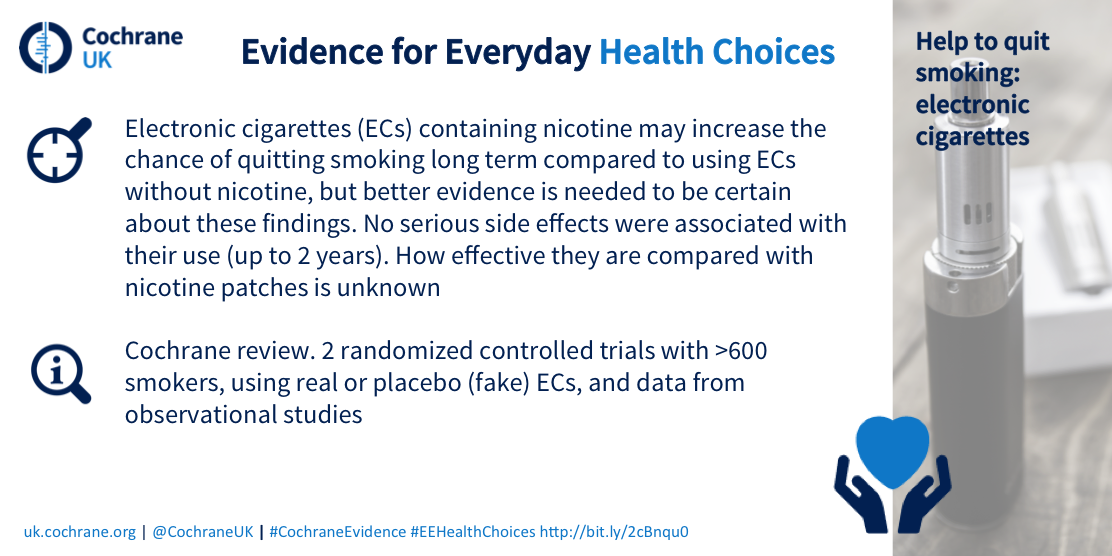
An updated Cochrane Review provides an independent, rigorous assessment of the best available evidence to date about electronic cigarettes for quitting smoking.
Scroll to the bottom of this article for a round-up of media coverage
The conclusions of this updated Review are unchanged since the last review was published two years ago: electronic cigarettes may help smokers stop their smoking, and the included studies did not find any serious side effects associated with their use for up to two years.
Many studies are now underway which may help us understand more about their effects in the future.
The first Cochrane Review, published in the Cochrane Library in December 2014, showed that electronic cigarettes may be an aid to smokers in stopping their smoking. The updated Review did not find any new randomized controlled trials (RCTs) with long-term outcomes looking at the effectiveness of electronic cigarettes in helping people to stop smoking. However, this is an active area of research, with a large number of ongoing studies that will add to the evidence in the next few years.
Smoking is a significant global health problem. Despite many smokers wanting to stop, they often find it difficult to succeed in the long term. One of the most effective and widely used strategies to help combat the cravings associated with nicotine addiction is to deliver nicotine by patches and chewing gum.
Electronic cigarettes have been around in some form for a number of years, but over the past few years their popularity has increased significantly, and they have begun to look and feel less like conventional cigarettes. Unlike chewing gum and patches, they mimic the experience of cigarette smoking because they are hand-held and generate a smoke-like vapour when used. They help to recreate similar sensations of smoking without exposing users or others to the smoke from conventional cigarettes, and can be used to provide smokers with nicotine. Though they are used by many smokers, little is still known about how effective they are at helping people stop smoking.
This version of the updated Cochrane Review includes no new RCTs. The original Review included two RCTs involving more than 600 participants, and found that electronic cigarettes containing nicotine may increase the chances of stopping smoking within six to 12 months, compared to using an electronic cigarette without nicotine. The researchers could not determine whether using electronic cigarettes was better than a nicotine patch in helping people stop smoking, because there were not enough people taking part in the study.
This updated Review now includes observational data from an additional 11 studies. Of the studies which measured side effects, none found any serious side effects of using electronic cigarettes for up to two years. The studies showed that throat and mouth irritation are the most commonly reported side effects in the short to medium term (up to two years).
The lead author of this Cochrane Review, Jamie Hartmann-Boyce from the Cochrane Tobacco Addiction Group, said, “The randomized evidence on smoking cessation is unchanged since the last version of the Review. We are encouraged to find many studies are now underway, particularly as electronic cigarettes are an evolving technology. Since the last version of the Review, 11 new observational and uncontrolled studies have been published. In terms of quitting, these can’t provide the same information we get from randomized controlled trials, but they contribute further information on the side effects of using electronic cigarettes to quit smoking. None detected any serious side effects, but longer term data are needed.”
Read this Press Release in French, Spanish or Polish .
Editor’s notes Full citation: Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation . Cochrane Database of Systematic Reviews 2016, Issue 9. Art. No.: CD010216. DOI: 10.1002/14651858.CD010216.pub3.
Cochrane Review Author contact details : [email protected]
For all media enquiries, please contact:
Jo Anthony Senior Media and Communications Officer, Cochrane M +44(0) 7582 726 634 E [email protected] or [email protected]
About Cochrane Cochrane is a global independent network of researchers, professionals, patients, carers, and people interested in health. Cochrane produces reviews which study all of the best available evidence generated through research and make it easier to inform decisions about health. These are called systematic reviews. Cochrane is a not-for-profit organization with collaborators from more than 130 countries working together to produce credible, accessible health information that is free from commercial sponsorship and other conflicts of interest. Our work is recognized as representing an international gold standard for high quality, trusted information.
Find out more at cochrane.org | Follow us on twitter @cochranecollab
If you are a journalist or member of the press and wish to receive news alerts before their online publication or if you wish to arrange an interview with an author, please contact the Cochrane press office: [email protected]
About Wiley Wiley is a global provider of knowledge and knowledge-enabled services that improve outcomes in areas of research, professional practice, and education. Through the Research segment, the Company provides digital and print scientific, technical, medical, and scholarly journals, reference works, books, database services, and advertising. The Professional Development segment provides digital and print books, online assessment and training services, and test prep and certification. In Education, Wiley provides education solutions including online program management services for higher education institutions and course management tools for instructors and students, as well as print and digital content. The Company's website can be accessed at http://www.wiley.com .
Selected Media Coverage:
E-cigarettes can help smokers quit, says study in The Guardian . Why can't scientists agree on e-cigarettes? blog post in The Guardian . E-Cigs Might Help Some Quit Smoking, New Study Reveals on Consumer Reports .

Public Health Consequences of E-Cigarettes (2018)
Chapter: summary.
E-cigarette aerosol contains fewer numbers and lower levels of most toxicants than does smoke from combustible tobacco cigarettes. Exposure to nicotine and to toxicants from the aerosolization of e-cigarette ingredients is dependent on user and device characteristics. Laboratory tests of e-cigarette ingredients, in vitro toxicological tests, and short-term human studies suggest that e-cigarettes are likely to be far less harmful than combustible tobacco cigarettes. However, the absolute risks of the products cannot be unambiguously determined at this time. Long-term health effects, of particular concern for youth who become dependent on such products, are not yet clear.
Although e-cigarette use might cause youth to transition to combustible tobacco products, it might also increase adult cessation of combustible tobacco cigarettes. The net public health effect, harm or benefit, of e-cigarettes depends on three factors: their effect on youth initiation of combustible tobacco products, their effect on adult cessation of combustible tobacco products, and their intrinsic toxicity. If e-cigarette use by adult smokers leads to long-term abstinence from combustible tobacco cigarettes, the benefit to public health could be considerable. Without that health benefit for adult smokers, e-cigarette use could cause considerable harm to public health in the short and long term due both to the inherent harms of exposure to e-cigarette toxicants and to the harms related to subsequent combustible tobacco use by those who begin using e-cigarettes in their youth.
Population modeling is a useful strategy to help estimate the balance of potential benefits and harms from e-cigarettes in the short term before more definite scientific data are available. Factors that would promote the potential health benefits associated with these products include determining with more precision
under which conditions e-cigarettes could serve as an effective smoking cessation aid, discouraging their use among youth through tobacco control strategies such as education and restrictions on products particularly appealing to youth, and increasing their safety through data-driven product engineering and design.
Millions of Americans use electronic cigarettes (e-cigarettes), even as rates of smoking 1 combustible tobacco cigarettes continue to decline among youth and adults. In 2016, youth e-cigarette use was substantially higher than cigarette smoking or use of any other tobacco product. A common picture emerges from national surveys. Prevalence of use increases with age in children and youth. E-cigarette use also varies by gender, with typically greater use among boys than girls. E-cigarette use also varies by race and ethnicity, with higher rates of use among youth who identify as Hispanic and non-Hispanic white compared with black, Asian, and other races. Early results suggest that use stabilized or decreased in youth between 2015 and 2016, despite increases between 2011 and 2015 across a range of measures and surveys. Substantial proportions of youth report using non-nicotine electronic cigarettes. Rates of e-cigarette use among adults are relatively low when compared with youth e-cigarette use and to adult combustible tobacco cigarette smoking. Most adult e-cigarette users report currently using other tobacco products. Among adults, as among youth, patterns of use vary by demographic subgroups—age, gender, and race and ethnicity. E-cigarette use is generally greatest among young adults and decreases with age in adults. Few adults begin using e-cigarettes who are not already using combustible tobacco cigarettes.
Despite their popularity, little is known about their health effects, and perceptions of potential risks and benefits of e-cigarette use vary widely among the public, users of e-cigarettes, health care providers, and the public health community. For example, whether e-cigarette use confers lower risk of addiction compared with combustible tobacco cigarettes is one point of controversy. Electronic cigarettes contain constituents that are not inert and are likely to have some negative health effects on their own. However, because the known risks of combustible tobacco are so great, understanding the net public health effect of e-cigarettes requires understanding not only the inherent risks of e-cigarettes, but also the relationship between e-cigarette use and combustible tobacco cigarette use.
Furthermore, concerns have been raised that e-cigarettes will induce youth to begin using combustible tobacco cigarettes. E-cigarette use among youth and young adults is especially worrying if e-cigarettes cause
___________________
1 The committee uses the verb “smoke” to refer to use of combustible tobacco cigarettes and “vape” to refer to use of e-cigarettes. Similarly “smoker” refers to someone who uses combustible tobacco cigarettes.
dependence or the normalization of smoking behavior, and subsequently lead youth and young adults to start smoking combustible tobacco cigarettes. This is of particular concern for youth who otherwise would never have smoked. Among adult populations, to the extent that e-cigarette use promotes either reduction or complete abstinence from combustible tobacco smoking, e-cigarettes may help to reduce health risks.
E-cigarettes are regulated as tobacco products 2 by the Center for Tobacco Products of the Food and Drug Administration (FDA), which requested that the National Academies of Sciences, Engineering, and Medicine convene a committee of experts to conduct a review of the emerging evidence about e-cigarettes and health, make recommendations for the improvement of this research, and highlight gaps that are a priority for future research. The Statement of Task can be found in Box S-1 .
The committee undertook a comprehensive review of the scientific literature regarding key constituents in e-cigarettes, human health effects, initiation and cessation of combustible tobacco cigarette use, and harm reduction. The committee considered the quality of individual studies, as well as the totality of the evidence to provide structured and consistent conclusions on the strength of the evidence. See Box S-2 for a summary of the framework the committee used for those conclusions. The committee notes that the framework is a guide, but that a great deal of expert judgment—in the evaluation of individual studies and in bodies of evidence—is always involved. The Annex to this Summary includes a compilation of the conclusions grouped by level of evidence, whereas they are listed by type of outcome in the sections that follow.
CONSTITUENTS
E-cigarettes contain liquids (referred to as e-liquids) that are aerosolized upon operation of the device. E-liquids typically contain nicotine (although some users prefer zero-nicotine solutions), flavorings, and humectants. Nicotine is a well-understood compound with known central and peripheral nervous system effects. It causes dependence and addiction, and exposure to nicotine from e-cigarettes likely elevates the cardiovascular disease risk in people with pre-existing cardiovascular disease(s), but the cardiovascular risk in people without cardiovascular disease(s) is uncertain. Based on studies of long-term users of nicotine replacement
2 If an e-cigarette manufacturer made a claim in packaging or advertising that the products were useful for smoking cessation, the product would be regulated as a drug-delivery device under different statutory authorities and not by the Center for Tobacco Products. E-cigarettes are regulated as tobacco products because the nicotine in the e-liquids derives from tobacco plants. The Food and Drug Administration recently exerted authority over e-cigarettes; those that do not contain nicotine may be reviewed on a case-by-case basis.
therapy or smokeless tobacco, nicotine exposure from e-cigarette use will likely pose minimal cancer risk to users. Most flavorings in e-liquids are designated as generally recognized as safe (also known as GRAS) by FDA, but those designations are for oral consumption in food and do not apply to flavorings used in e-cigarettes; most of these were never studied for toxicity via the inhalation route. The primary humectants are propylene glycol and glycerol, compounds also in widespread use for other purposes and about which significant scientific literature exists.
In reviewing the literature about the constituents in and exposures from e-cigarettes, the committee made nine conclusions:
Conclusion 3-1. There is conclusive evidence that e-cigarette use increases airborne concentrations of particulate matter and nicotine in indoor environments compared with background levels.
Conclusion 3-2. There is limited evidence that e-cigarette use increases levels of nicotine and other e-cigarette constituents on a variety of indoor surfaces compared with background levels.
Conclusion 4-1. There is conclusive evidence that exposure to nicotine from e-cigarettes is highly variable and depends on product characteristics (including device and e-liquid characteristics) and how the device is operated.
Conclusion 4-2. There is substantial evidence that nicotine intake from e-cigarette devices among experienced adult e-cigarette users can be comparable to that from combustible tobacco cigarettes.
Conclusion 5-1. There is conclusive evidence that in addition to nicotine, most e-cigarette products contain and emit numerous potentially toxic substances.
Conclusion 5-2. There is conclusive evidence that, other than nicotine, the number, quantity, and characteristics of potentially toxic substances emitted from e-cigarettes are highly variable and depend on product characteristics (including device and e-liquid characteristics) and how the device is operated.
Conclusion 5-3. There is substantial evidence that except for nicotine, under typical conditions of use, exposure to potentially toxic substances from e-cigarettes is significantly lower compared with combustible tobacco cigarettes.
Conclusion 5-4. There is substantial evidence that e-cigarette aerosol contains metals. The origin of the metals could be the metallic coil used to heat the e-liquid, other parts of the e-cigarette device, or e-liquids. Product characteristics and use patterns may contribute to differences in the actual metals and metal concentrations measured in e-cigarette aerosol.
Conclusion 5-5. There is limited evidence that the number of metals in e-cigarette aerosol could be greater than the number of metals in combustible tobacco cigarettes, except for cadmium, which is markedly lower in e-cigarettes compared with combustible tobacco cigarettes.
Taken together, the evidence in support of these conclusions suggests that e-cigarette aerosol contains fewer numbers and lower levels of toxicants than smoke from combustible tobacco cigarettes. Nicotine exposure can mimic that found with use of combustible tobacco cigarettes, but is highly variable. However, the exposure to nicotine and toxicants from the aerosolization of flavorings and humectants is dependent on user and device characteristics.
HUMAN HEALTH EFFECTS
Combustible tobacco cigarettes pose serious risks to human health; these risks are well documented and well understood. Many of those health effects emerge only after decades of cigarette smoking. E-cigarettes have only been on the market in the United States since 2006, making scientific comparisons between e-cigarettes and combustible tobacco cigarettes about most health effects difficult. However, research on short-term exposures to e-cigarettes and effects on disease symptoms and intermediate outcomes exist. An important distinction when considering these data
is whether the effects are seen in an e-cigarette user who had never used combustible tobacco cigarettes (usually children or youth) or in a combustible tobacco cigarette user, with and without preexisting tobacco-related disease, usually adults. The committee reviewed evidence on the effects of e-cigarettes in several health domains: dependence, cardiovascular disease, cancer, respiratory diseases, oral diseases, maternal and fetal outcomes, and injuries and poisonings. Although the amount of literature is relatively scant and complicated by the multiple types of e-cigarettes in use even within a given study, the committee made 26 conclusions about the effects of e-cigarettes on health.
Conclusion 7-1. There is substantial evidence that e-cigarette aerosols can induce acute endothelial cell dysfunction, although the long-term consequences and outcomes on these parameters with long-term exposure to e-cigarette aerosol are uncertain.
Conclusion 7-2. There is substantial evidence that components of e-cigarette aerosols can promote formation of reactive oxygen species/oxidative stress. Although this supports the biological plausibility of tissue injury and disease from long-term exposure to e-cigarette aerosols, generation of reactive oxygen species and oxidative stress induction is generally lower from e-cigarettes than from combustible tobacco cigarette smoke.
Conclusion 8-1. There is substantial evidence that e-cigarette use results in symptoms of dependence on e-cigarettes.
Conclusion 8-2. There is moderate evidence that risk and severity of dependence are lower for e-cigarettes than combustible tobacco cigarettes.
Conclusion 8-3. There is moderate evidence that variability in e-cigarette product characteristics (nicotine concentration, flavoring, device type, and brand) is an important determinant of risk and severity of e-cigarette dependence.
Conclusion 9-1. There is no available evidence whether or not e-cigarette use is associated with clinical cardiovascular outcomes (coronary heart disease, stroke, and peripheral artery disease) and subclinical atherosclerosis (carotid intima-media thickness and coronary artery calcification).
Conclusion 9-2. There is substantial evidence that heart rate increases shortly after nicotine intake from e-cigarettes.
Conclusion 9-3. There is moderate evidence that diastolic blood pressure increases shortly after nicotine intake from e-cigarettes.
Conclusion 9-4. There is limited evidence that e-cigarette use is associated with a short-term increase in systolic blood pressure, changes in biomarkers of oxidative stress, increased endothelial dysfunction and arterial stiffness, and autonomic control.
Conclusion 9-5. There is insufficient evidence that e-cigarette use is associated with long-term changes in heart rate, blood pressure, and cardiac geometry and function.
Conclusion 10-1. There is no available evidence whether or not e-cigarette use is associated with intermediate cancer endpoints in humans. This holds true for e-cigarette use compared with use of combustible tobacco cigarettes and e-cigarette use compared with no use of tobacco products.
Conclusion 10-2. There is limited evidence from in vivo animal studies using intermediate biomarkers of cancer to support the hypothesis that long-term e-cigarette use could increase the risk of cancer; there is no available evidence from adequate long-term animal bioassays of e-cigarette aerosol exposures to inform cancer risk.
Conclusion 10-3. There is limited evidence that e-cigarette aerosol can be mutagenic or cause DNA damage in humans, animal models, and human cells in culture.
Conclusion 10-4. There is substantial evidence that some chemicals present in e-cigarette aerosols (e.g., formaldehyde, acrolein) are capable of causing DNA damage and mutagenesis. This supports the biological plausibility that long-term exposure to e-cigarette aerosols could increase risk of cancer and adverse reproductive outcomes. Whether or not the levels of exposure are high enough to contribute to human carcinogenesis remains to be determined.
Conclusion 11-1. There is no available evidence whether or not e-cigarettes cause respiratory diseases in humans.
Conclusion 11-2. There is limited evidence for improvement in lung function and respiratory symptoms among adult smokers with asthma who switch to e-cigarettes completely or in part (dual use).
Conclusion 11-3. There is limited evidence for reduction of chronic obstructive pulmonary disease (COPD) exacerbations among adult smokers with COPD who switch to e-cigarettes completely or in part (dual use).
Conclusion 11-4. There is moderate evidence for increased cough and wheeze in adolescents who use e-cigarettes and an association with e-cigarette use and an increase in asthma exacerbations.
Conclusion 11-5. There is limited evidence of adverse effects of e-cigarette exposure on the respiratory system from animal and in vitro studies.
Conclusion 12-1. There is limited evidence suggesting that switching to e-cigarettes will improve periodontal disease in smokers.
Conclusion 12-2. There is limited evidence suggesting that nicotine- and non-nicotine–containing e-cigarette aerosol can adversely affect cell viability and cause cell damage of oral tissue in non-smokers.
Conclusion 13-1. There is no available evidence whether or not e-cigarettes affect pregnancy outcomes.
Conclusion 13-2. There is insufficient evidence whether or not maternal e-cigarette use affects fetal development.
Conclusion 14-1. There is conclusive evidence that e-cigarette devices can explode and cause burns and projectile injuries. Such risk is significantly increased when batteries are of poor quality, stored improperly, or modified by users.
Conclusion 14-2. There is conclusive evidence that intentional or accidental exposure to e-liquids (from drinking, eye contact, or dermal contact) can result in adverse health effects including but not limited to seizures, anoxic brain injury, vomiting, and lactic acidosis.
Conclusion 14-3. There is conclusive evidence that intentionally or unintentionally drinking or injecting e-liquids can be fatal.
Taken together, the evidence reviewed by the committee suggests that e-cigarettes are not without physiological activity in humans, but the implications for long-term effects on morbidity and mortality are not yet clear. Use of e-cigarettes instead of combustible tobacco cigarettes by those with existing respiratory disease might be less harmful.
INITIATION AND CESSATION
The Family Smoking Prevention and Tobacco Control Act of 2009, which is the basis for FDA’s regulatory authority over tobacco products,
including e-cigarettes, defined a unique regulatory standard, the public health standard. This requires that tobacco products introduced on the market after February 15, 2007, be shown to have a net population health benefit to users and non-users of the product. Operationally, if a product caused more people to begin harmful tobacco use and fewer people to quit tobacco use, even if the product itself poses less risk to the user than other products, it could be determined that the product poses a public health burden and would be kept off the market. Thus, the tobacco control field must pay close attention to the effects of e-cigarette use on initiation and cessation of combustible tobacco use, regardless of the effects of e-cigarettes on health outcomes. Although the studies reviewed had limitations, the committee was able to make seven conclusions:
Conclusion 16-1. There is substantial evidence that e-cigarette use increases risk of ever using combustible tobacco cigarettes among youth and young adults.
Conclusion 16-2. Among youth and young adult e-cigarette users who ever use combustible tobacco cigarettes, there is moderate evidence that e-cigarette use increases the frequency and intensity of subsequent combustible tobacco cigarette smoking.
Conclusion 16-3. Among youth and young adult e-cigarette users who ever use combustible tobacco cigarettes, there is limited evidence that e-cigarette use increases, in the near term, the duration of subsequent combustible tobacco cigarette smoking.
Conclusion 17-1. Overall, there is limited evidence that e-cigarettes may be effective aids to promote smoking cessation.
Conclusion 17-2. There is moderate evidence from randomized controlled trials that e-cigarettes with nicotine are more effective than e-cigarettes without nicotine for smoking cessation.
Conclusion 17-3. There is insufficient evidence from randomized controlled trials about the effectiveness of e-cigarettes as cessation aids compared with no treatment or to Food and Drug Administration–approved smoking cessation treatments.
Conclusion 17-4. While the overall evidence from observational trials is mixed, there is moderate evidence from observational studies that more frequent use of e-cigarettes is associated with an increased likelihood of cessation.
Taken together the evidence suggests that while e-cigarettes might cause youth who use them to transition to use of combustible tobacco products, they might increase adult cessation of combustible tobacco cigarettes.
HARM REDUCTION
The committee reviewed evidence from the sections discussed above to specifically look at what is known about e-cigarette exposures and health effects when compared with combustible tobacco cigarettes. The committee reached five conclusions.
Conclusion 18-1. There is conclusive evidence that completely substituting e-cigarettes for combustible tobacco cigarettes reduces users’ exposure to numerous toxicants and carcinogens present in combustible tobacco cigarettes.
Conclusion 18-2. There is substantial evidence that completely switching from regular use of combustible tobacco cigarettes to e-cigarettes results in reduced short-term adverse health outcomes in several organ systems.
Conclusion 18-3. There is no available evidence whether or not long-term e-cigarette use among smokers (dual use) changes morbidity or mortality compared with those who only smoke combustible tobacco cigarettes.
Conclusion 18-4. There is insufficient evidence that e-cigarette use changes short-term adverse health outcomes in several organ systems in smokers who continue to smoke combustible tobacco cigarettes (dual users).
Conclusion 18-5. There is moderate evidence that secondhand exposure to nicotine and particulates is lower from e-cigarettes compared with combustible tobacco cigarettes.
The evidence about harm reduction suggests that across a range of studies and outcomes, e-cigarettes pose less risk to an individual than combustible tobacco cigarettes.
The committee used population dynamic modeling to examine the possible effects of e-cigarette use at the population level. The specific time frame and magnitude of population health effects of e-cigarettes will depend on their impact on the rates of initiation and cessation of combus-
tible tobacco cigarettes and on their intrinsic harm. Any population health effect includes the possibility of some groups incurring harm (e.g., youth who initiate smoking combustible tobacco cigarettes), while others benefit (e.g., adult combustible tobacco cigarette users who completely quit or reduce smoking). As with other models of population health effects of tobacco use, the effects of changing cessation rates are seen earlier than effects of changing initiation rates, due to the lag time for serious chronic health effects of combustible tobacco cigarettes to manifest.
Under the assumption that the use of e-cigarettes increases the net cessation rate of combustible tobacco cigarette use among adults (i.e., the increase in permanent quitting offsets the potential relapse of former smokers because of e-cigarettes), the modeling projects that use of these products will generate a net public health benefit, at least in the short run. The harms from increased initiation by youth will take time to manifest, occurring decades after the benefits of increased cessation are seen. However, for long-range projections (e.g., 50 years out), the net public health benefit is substantially less and is negative under some scenarios. With the range of assumptions used, the model projects that there would be net public health harm in the short and long terms if the products do not increase combustible tobacco cessation in adults.
Factors that would maximize potential health benefits associated with these products include determining with more precision whether and under which conditions e-cigarettes could serve as an effective smoking cessation aid, discouraging their use among youth through standard tobacco control strategies such as education and access restrictions, and increasing their safety through data-driven product engineering and design.
RESEARCH RECOMMENDATIONS
Given the relatively short time that e-cigarettes have been used, it is understandable that the evidence base regarding their effects is limited. There is a great need for more evidence. Manufacturers will need to produce this research in a short amount of time if current statutory deadlines remain in place. Researchers from academia will also be involved directly (in contracts with manufacturers and in grants from government and others) in the generation of these data. Some types of research involve a long-term horizon; other important and informative research requires much less time to conduct. One type of research does not substitute for the other; a complete portfolio of research is needed. The committee understands that, in any new field, researchers struggle to conduct optimal research due to limitations of knowledge. Also, researchers feel the urgency to study an important new question and adapt what they know,
without complete adjustments in research design or methods sufficient to address the nuances of the problem. Finally, the rapidly changing nature of the devices has made comparisons among studies difficult.
The committee identified gaps in the literature in every aspect in its work and provides overarching categories of research needs and specific research suggestions within the final chapters of each of the three major sections of the report. These overarching categories include (1) address-
ing gaps in substantive knowledge and (2) improving research methods and quality through protocol and methods validation and development, including the use of appropriate study design. The six specific research recommendations and select suggestions can be found in Boxes S-3 , S-4 ,
and S-5 . The specific suggestions illustrate the range of priority research areas provided in the body of the report.
FINAL OBSERVATIONS
Much of the research on e-cigarettes suffers from methodological flaws, and many important areas have not yet been researched. Nonetheless, the committee found sufficient literature to suggest that, while there are risks associated with e-cigarettes, compared with combustible tobacco cigarettes, e-cigarettes contain fewer toxicants; can deliver nicotine in a manner similar to combustible tobacco cigarettes; show significantly less
biological activity in a number of in vitro, animal, and human systems; and might be useful as a cessation aid to smokers who use e-cigarettes exclusively. However, youth who begin with e-cigarettes are more likely to transition to combustible tobacco cigarette use and become smokers who may be at risk to suffer the known health burdens of combustible tobacco cigarettes. Moreover, although infrequent, e-cigarettes can explode, leading to burns and other injuries, and consumption of or dermal exposure to e-liquids is dangerous, even fatal.
More and better research on short- and long-term health effects of e-cigarettes, as well as their effects on initiation and cessation of combustible tobacco product use, will bring clarity to the question of whether e-cigarettes will prove to reduce harm or induce harm at the individual and the population levels. Given how rapidly the e-cigarette product marketplace and user population are changing, there will undoubtedly be many new issues, which are currently unknown and will require careful surveillance and scientific scrutiny. The approach taken by the committee to evaluate the health effects of e-cigarettes in this report is anticipated to provide a generalizable template for future evaluations of the evidence.
Millions of Americans use e-cigarettes. Despite their popularity, little is known about their health effects. Some suggest that e-cigarettes likely confer lower risk compared to combustible tobacco cigarettes, because they do not expose users to toxicants produced through combustion. Proponents of e-cigarette use also tout the potential benefits of e-cigarettes as devices that could help combustible tobacco cigarette smokers to quit and thereby reduce tobacco-related health risks. Others are concerned about the exposure to potentially toxic substances contained in e-cigarette emissions, especially in individuals who have never used tobacco products such as youth and young adults. Given their relatively recent introduction, there has been little time for a scientific body of evidence to develop on the health effects of e-cigarettes.
Public Health Consequences of E-Cigarettes reviews and critically assesses the state of the emerging evidence about e-cigarettes and health. This report makes recommendations for the improvement of this research and highlights gaps that are a priority for future research.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Note : This news story is more than five years old .

Image credit: Oleg Baliuk/ Shutterstock
Conclusions about the effects of electronic cigarettes remain the same
An updated Cochrane Review, led by a University of Oxford researcher, provides an independent, rigorous assessment of the best available evidence to date about electronic cigarettes for quitting smoking. The conclusions of this updated Review are unchanged since the last review was published two years ago: electronic cigarettes may help smokers stop their smoking, and the included studies did not find any serious side effects associated with their use for up to two years.
We are encouraged to find many studies are now underway, particularly as e-cigarettes are an evolving technology. Jamie Hartmann-Boyce, Nuffield Department of Primary Care Health Sciences
We are encouraged to find many studies are now underway, particularly as electronic cigarettes are an evolving technology.
The first Cochrane Review, published in the Cochrane Library in December 2014, showed that electronic cigarettes may be an aid to smokers in stopping their smoking. The updated Review did not find any new randomized controlled trials (RCTs) with long-term outcomes looking at the effectiveness of electronic cigarettes in helping people to stop smoking. However, this is an active area of research, with a large number of ongoing studies that will add to the evidence in the next few years.
Smoking is a significant global health problem. Despite many smokers wanting to stop, they often find it difficult to succeed in the long-term. One of the most effective and widely used strategies to help combat the cravings associated with nicotine addiction is to deliver nicotine by patches and chewing gum.
Electronic cigarettes have been around in some form for a number of years, but over the past few years their popularity has increased significantly, and they have begun to look and feel less like conventional cigarettes. Unlike chewing gum and patches, they mimic the experience of cigarette smoking because they are hand-held and generate a smoke-like vapour when used. They help to recreate similar sensations of smoking without exposing users or others to the smoke from conventional cigarettes, and can be used to provide smokers with nicotine. Though they are used by many smokers, little is still known about how effective they are at helping people stop smoking.
This version of the updated Cochrane Review includes no new RCTs. The original Review included two RCTs involving more than 600 participants, and found that electronic cigarettes containing nicotine may increase the chances of stopping smoking within six to 12 months, compared to using an electronic cigarette without nicotine. The researchers could not determine whether using electronic cigarettes was better than a nicotine patch in helping people stop smoking, because there were not enough people taking part in the study.
This updated Review now includes observational data from an additional 11 studies. Of the studies which measured side effects, none found any serious side effects of using electronic cigarettes for up to two years. The studies showed that throat and mouth irritation are the most commonly reported side effects in the short-to medium-term (up to two years).
The lead author, Jamie Hartmann-Boyce from the Cochrane Tobacco Addiction Group, said, 'The randomized evidence on smoking cessation is unchanged since the last version of the Review. We are encouraged to find many studies are now underway, particularly as electronic cigarettes are an evolving technology. Since the last version of the Review, 11 new observational and uncontrolled studies have been published. In terms of quitting, these can’t provide the same information we get from randomized controlled trials, but they contribute further information on the side effects of using electronic cigarettes to quit smoking. None detected any serious side effects, but longer term data are needed.'
Further information
- Cochrane Review of E-Cigarettes
Researchers
- Jamie Hartmann-Boyce
- Nuffield Department of Primary Care Health Sciences
DISCOVER MORE
- Support Oxford's research
- Partner with Oxford on research
- Study at Oxford
- Research jobs at Oxford
You can view all news or browse by category

How bad is vaping and should it be banned?
Professor at the National Drug Research Institute (Melbourne), Curtin University
PhD Candidate (Psychiatry) & Research Assistant, University of Newcastle
Disclosure statement
Nicole Lee works as a consultant in the health sector and a psychologist in private practice. She has previously received funding by Australian and state governments, NHMRC and other bodies for evaluation and research into alcohol and other drug prevention and treatment.
Brigid Clancy is an Associate at 360Edge, a drug and alcohol consultancy company.
University of Newcastle and Curtin University provide funding as members of The Conversation AU.
View all partners
Vaping regularly makes headlines, with some campaigning to make e-cigarettes more available to help smokers quit, while others are keen to see vaping products banned, citing dangers, especially for teens.
So just how dangerous is it? We have undertaken an evidence check of vaping research . This included more than 100 sources on tobacco harm reduction, vaping prevalence and health effects, and what other countries are doing in response. Here’s what we found.
How does vaping compare to smoking?
Smoking is harmful. It’s the leading preventable cause of death in Australia. It causes 13% of all deaths , including from lung, mouth, throat and bladder cancer, emphysema, heart attack and stroke, to name just a few. People who smoke regularly and don’t quit lose about ten years of life compared with non-smokers.
Nicotine, a mild stimulant, is the active ingredient in both cigarettes and nicotine vaping products. It’s addictive but isn’t the cause of cancer or the other diseases related to smoking.
Ideally, people wouldn’t be addicted to nicotine, but having a safe supply without the deadly chemicals, for instance by using nicotine patches or gum, is safer than smoking. Making these other sources available is known as “harm reduction”.
Vaping is not risk-free, but several detailed reviews of the evidence plus a consensus of experts have all estimated it’s at least 95% safer to vape nicotine than to smoke tobacco. The risk of cancer from vaping, for example, has been estimated at less than 1%.
These reviews looked at the known dangerous chemicals in cigarettes, and found there were very few and in very small quantities in nicotine vapes. So the argument that we won’t see major health effects for a few more decades is causing more alarm than is necessary.

Is ‘everyone’ vaping these days?
Some are concerned about the use of vaping products by teens, but currently available statistics show very few teens vape regularly. Depending on the study, between 9.6% and 32% of 14-17-year-olds have tried vaping at some point in their lives.
But less than 2% of 14-17-year-olds say they have used vapes in the past year. This number doubled between 2016 and 2019, but is still much lower than the rates of teen smoking (3.2%) and teen alcohol use (32%).
It’s the same pattern we see with drugs other than alcohol: a proportion of people try them but only a very small proportion of those go on to use regularly or for a long time. Nearly 60% of people who try vaping only use once or twice .
Smoking rates in Australia have declined from 24% in 1991 to 11% in 2019 because we have introduced a number of very successful measures such as restricting sales and where people can smoke, putting up prices, introducing plain packaging, and improving education and access to treatment programs.
But it’s getting harder to encourage the remaining smokers to quit with the methods that have worked in the past. Those still smoking tend to be older , more socially disadvantaged , or have mental health problems.
Read more: My teen's vaping. What should I say? 3 expert tips on how to approach 'the talk'
Should we ban vapes?
So we have a bit of a dilemma. Vaping is much safer than smoking, so it would be helpful for adults to have access to it as an alternative to cigarettes. That means we need to make them more available and accessible.
But ideally we don’t want teens who don’t already smoke to start regular vaping. This has led some to call for a “ crackdown ” on vaping.
But we know from a long history of drug prohibition - like alcohol prohibition in the 1920s - that banning or restricting vaping could actually do more harm than good.
Banning drugs doesn’t stop people using them - more than 43% of Australians have tried an illicit drug at least once. And it has very little impact on the availability of drugs.
But prohibition does have a number of unintended consequences, including driving drugs underground and creating a black market or increasing harms as people switch to other drugs, which are often more dangerous.
The black market makes drugs more dangerous because there is no way to control quality. And it makes it easier, not harder, for teens to access them, because there are no restrictions on who can sell or buy them.
Read more: Learning about the health risks of vaping can encourage young vapers to rethink their habit
Are our current laws working?
In 2021, Australia made it illegal to possess and use nicotine vaping products without a prescription. We are the only country in the world to take this path.
The problem is even after more than a year of this law, only 8.6% of people vaping nicotine have a prescription, meaning more than 90% buy them illegally.
Anecdotal reports even suggest an increase in popularity of vaping among teens since these laws were introduced. At best, they are not helping.
It may seem counterintuitive, but the way to reduce the black market is to make quality-controlled vapes and liquids more widely available, but restricted to adults. If people could access vaping products legally they wouldn’t buy them on the black market and the black market would decline.
We also know from many studies on drug education in schools that when kids get accurate, non-sensationalised information about drugs they tend to make healthier decisions. Sensationalised information can have the opposite effect and increase interest in drugs . So better education in schools and for parents and teachers is also needed, so they know how to talk to kids about vaping and what to do if they know someone is vaping.
What have other countries done?
Other countries allow vapes to be legally sold without a prescription, but impose strict quality controls and do not allow the sale of products to people under a minimum age. This is similar to our regulation of cigarettes and alcohol.
The United Kingdom has minimum standards on manufacturing, as well as restrictions on purchase age and where people can vape.
Aotearoa New Zealand introduced a unique plan to reduce smoking rates by imposing a lifetime ban on buying cigarettes. Anyone born after January 1 2009 will never be able to buy cigarettes, so the minimum age you can legally smoke keeps increasing. At the same time, NZ increased access to vaping products under strict regulations on manufacture, purchase and use.
As of late last year, all US states require sellers to have a retail licence, and sales to people under 21 are banned. There are also restrictions on where people can vape.
A recent study modelled the impact of increasing access to nicotine vaping products in Australia. It found it’s likely there would be significant public health benefits by relaxing the current restrictive policies and increasing access to nicotine vaping products for adults.
The question is not whether we should discourage teens from using vaping products or whether we should allow wider accessibility to vaping products for adults as an alternative to smoking. The answer to both those questions is yes.
The key question is how do we do both effectively without one policy jeopardising the outcomes of the other?
If we took a pragmatic harm-reduction approach, as other countries have done, we could use our very successful model of regulation of tobacco products as a template to achieve both outcomes.
Read more: It's safest to avoid e-cigarettes altogether – unless vaping is helping you quit smoking
- Tobacco control

Service Delivery Consultant

Newsletter and Deputy Social Media Producer

College Director and Principal | Curtin College

Head of School: Engineering, Computer and Mathematical Sciences

Educational Designer
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Impact of vaping on...
Impact of vaping on respiratory health
Linked editorial.
Protecting children from harms of vaping
- Related content
- Peer review
- Andrea Jonas , clinical assistant professor
- Division of Pulmonary, Allergy, and Critical Care, Department of Medicine, Stanford University, Stanford, CA, USA
- Correspondence to A Jonas andreajonas{at}stanford.edu
Widespread uptake of vaping has signaled a sea change in the future of nicotine consumption. Vaping has grown in popularity over the past decade, in part propelled by innovations in vape pen design and nicotine flavoring. Teens and young adults have seen the biggest uptake in use of vape pens, which have superseded conventional cigarettes as the preferred modality of nicotine consumption. Relatively little is known, however, about the potential effects of chronic vaping on the respiratory system. Further, the role of vaping as a tool of smoking cessation and tobacco harm reduction remains controversial. The 2019 E-cigarette or Vaping Use-Associated Lung Injury (EVALI) outbreak highlighted the potential harms of vaping, and the consequences of long term use remain unknown. Here, we review the growing body of literature investigating the impacts of vaping on respiratory health. We review the clinical manifestations of vaping related lung injury, including the EVALI outbreak, as well as the effects of chronic vaping on respiratory health and covid-19 outcomes. We conclude that vaping is not without risk, and that further investigation is required to establish clear public policy guidance and regulation.
Abbreviations
BAL bronchoalveolar lavage
CBD cannabidiol
CDC Centers for Disease Control and Prevention
DLCO diffusing capacity of the lung for carbon monoxide
EMR electronic medical record
END electronic nicotine delivery systems
EVALI E-cigarette or Vaping product Use-Associated Lung Injury
LLM lipid laden macrophages
THC tetrahydrocannabinol
V/Q ventilation perfusion
Introduction
The introduction of vape pens to international markets in the mid 2000s signaled a sea change in the future of nicotine consumption. Long the mainstay of nicotine use, conventional cigarette smoking was on the decline for decades in the US, 1 2 largely owing to generational shifts in attitudes toward smoking. 3 With the advent of vape pens, trends in nicotine use have reversed, and the past two decades have seen a steady uptake of vaping among young, never smokers. 4 5 6 Vaping is now the preferred modality of nicotine consumption among young people, 7 and 2020 surveys indicate that one in five US high school students currently vape. 8 These trends are reflected internationally, where the prevalence of vape products has grown in both China and the UK. 9 Relatively little is known, however, regarding the health consequences of chronic vape pen use. 10 11 Although vaping was initially heralded as a safer alternative to cigarette smoking, 12 13 the toxic substances found in vape aerosols have raised new questions about the long term safety of vaping. 14 15 16 17 The 2019 E-cigarette or Vaping product Use-Associated Lung Injury (EVALI) outbreak, ultimately linked to vitamin E acetate in THC vapes, raised further concerns about the health effects of vaping, 18 19 20 and has led to increased scientific interest in the health consequences of chronic vaping. This review summarizes the history and epidemiology of vaping, and the clinical manifestations and proposed pathophysiology of lung injury caused by vaping. The public health consequences of widespread vaping remain to be seen and are compounded by young users of vape pens later transitioning to combustible cigarettes. 4 21 22 Deepened scientific understanding and public awareness of the potential harms of vaping are imperative to confront the challenges posed by a new generation of nicotine users.
Sources and selection criteria
We searched PubMed and Ovid Medline databases for the terms “vape”, “vaping”, “e-cigarette”, “electronic cigarette”, “electronic nicotine delivery”, “electronic nicotine device”, “END”, “EVALI”, “lung injury, diagnosis, management, and treatment” to find articles published between January 2000 and December 2021. We also identified references from the Centers for Disease Control and Prevention (CDC) website, as well as relevant review articles and public policy resources. Prioritization was given to peer reviewed articles written in English in moderate-to-high impact journals, consensus statements, guidelines, and included randomized controlled trials, systematic reviews, meta-analyses, and case series. We excluded publications that had a qualitative research design, or for which a conflict of interest in funding could be identified, as defined by any funding source or consulting fee from nicotine manufacturers or distributors. Search terms were chosen to generate a broad selection of literature that reflected historic and current understanding of the effects of vaping on respiratory health.
The origins of vaping
Vaping achieved widespread popularity over the past decade, but its origins date back almost a century and are summarized in figure 1 . The first known patent for an “electric vaporizer” was granted in 1930, intended for aerosolizing medicinal compounds. 23 Subsequent patents and prototypes never made it to market, 24 and it wasn’t until 1979 that the first vape pen was commercialized. Dubbed the “Favor” cigarette, the device was heralded as a smokeless alternative to cigarettes and led to the term “vaping” being coined to differentiate the “new age” method of nicotine consumption from conventional, combustible cigarettes. 25 “Favor” cigarettes did not achieve widespread appeal, in part because of the bitter taste of the aerosolized freebase nicotine; however, the term vaping persisted and would go on to be used by the myriad products that have since been developed.

Timeline of vape pen invention to widespread use (1970s-2020)
- Download figure
- Open in new tab
- Download powerpoint
The forerunner of the modern vape pen was developed in Beijing in 2003 and later introduced to US markets around 2006. 26 27 Around this time, the future Juul Laboratories founders developed the precursor of the current Juul vape pen while they were students at the Stanford Byers-Center for Biodesign. 28 Their model included disposable cartridges of flavored nicotine solution (pods) that could be inserted into the vape pen, which itself resembled a USB flash drive. Key to their work was the chemical alteration of freebase nicotine to a benzoate nicotine salt. 29 The lower pH of the nicotine salt resulted in an aerosolized nicotine product that lacked a bitter taste, 30 and enabled manufacturers to expand the range of flavored vape products. 31 Juul Laboratories was founded a decade later and quickly rose to dominate the US market, 32 accounting for an estimated 13-59% of the vape products used among teens by 2020. 6 8 Part of the Juul vape pen’s appeal stems from its discreet design, as well as its ability to deliver nicotine with an efficiency matching that of conventional cigarettes. 33 34 Subsequent generations of vape pens have included innovations such as the tank system, which allowed users to select from the wide range of different vape solutions on the market, rather than the relatively limited selection available in traditional pod based systems. Further customizations include the ability to select different vape pen components such as atomizers, heating coils, and fluid wicks, allowing users to calibrate the way in which the vape aerosol is produced. Tobacco companies have taken note of the shifting demographics of nicotine users, as evidenced in 2018 by Altria’s $12.8bn investment in Juul Laboratories. 35
Vaping terminology
At present, vaping serves as an umbrella term that describes multiple modalities of aerosolized nicotine consumption. Vape pens are alternatively called e-cigarettes, electronic nicotine delivery systems (END), e-cigars, and e-hookahs. Additional vernacular terms have emerged to describe both the various vape pen devices (eg, tank, mod, dab pen), vape solution (eg, e-liquid, vape juice), as well as the act of vaping (eg, ripping, juuling, puffing, hitting). 36 A conventional vape pen is a battery operated handheld device that contains a storage chamber for the vape solution and an internal element for generating the characteristic vape aerosol. Multiple generations of vape pens have entered the market, including single use, disposable varieties, as well as reusable models that have either a refillable fluid reservoir or a disposable cartridge for the vape solution. Aerosol generation entails a heating coil that atomizes the vape solution, and it is increasingly popular for devices to include advanced settings that allow users to adjust features of the aerosolized nicotine delivery. 37 38 Various devices allow for coil temperatures ranging from 110 °C to over 1000 °C, creating a wide range of conditions for thermal degradation of the vape solution itself. 39 40
The sheer number of vape solutions on the market poses a challenge in understanding the impact of vaping on respiratory health. The spectrum of vape solutions available encompasses thousands of varieties of flavors, additives, and nicotine concentrations. 41 Most vape solutions contain an active ingredient, commonly nicotine 42 ; however, alternative agents include tetrahydrocannabinol (THC) or cannabidiol (CBD). Vape solutions are typically composed of a combination of a flavorant, nicotine, and a carrier, commonly propylene glycol or vegetable glycerin, that generates the characteristic smoke appearance of vape aerosols. Some 450 brands of vape now offer more than 8000 flavors, 41 a figure that nearly doubled over a three year period. 43 Such tremendous variety does not account for third party sellers who offer users the option to customize a vape solution blend. Addition of marijuana based products such as THC or CBD requires the use of an oil based vape solution carrier to allow for extraction of the psychoactive elements. Despite THC vaping use in nearly 9% of high schoolers, 44 THC vape solutions are subject to minimal market regulation. Finally, a related modality of THC consumption is termed dabbing, and describes the process of inhaling aerosolized THC wax concentrate.
Epidemiology of vaping
Since the early 2000s, vaping has grown in popularity in the US and elsewhere. 8 45 Most of the 68 million vape pen users are concentrated in China, the US, and Europe. 46 Uptake among young people has been particularly pronounced, and in the US vaping has overtaken cigarettes as the most common modality of nicotine consumption among adolescents and young adults. 47 Studies estimate that 20% of US high school students are regular vape pen users, 6 48 in contrast to the 5% of adults who use vape products. 2 Teen uptake of vaping has been driven in part by a perception of vaping as a safer alternative to cigarettes, 49 50 as well as marketing strategies that target adolescents. 33 Teen use of vape pens is further driven by the low financial cost of initiation, with “starter kits” costing less than $25, 51 as well as easy access through peer sales and inconsistent age verification at in-person and online retailers. 52 After sustained growth in use over the 2010s, recent survey data from 2020 suggest that the number of vape pen users has leveled off among teens, perhaps in part owing to increased perceived risk of vaping after the EVALI outbreak. 8 53 The public health implications of teen vaping are compounded by the prevalence of vaping among never smokers (defined as having smoked fewer than 100 lifetime cigarettes), 54 and subsequent uptake of cigarette smoking among vaping teens. 4 55 Similarly, half of adults who currently vape have never used cigarettes, 2 and concern remains that vaping serves as a gateway to conventional cigarette use, 56 57 although these results have been disputed. 58 59 Despite regulation limiting the sale of flavored vape products, 60 a 2020 survey found that high school students were still predominantly using fruit, mint, menthol, and dessert flavored vape solutions. 48 While most data available surround the use of nicotine-containing vape products, a recent meta-analysis showed growing prevalence of adolescents using cannabis-containing products as well. 61
Vaping as harm reduction
Despite facing ongoing questions about safety, vaping has emerged as a potential tool for harm reduction among cigarette smokers. 12 27 An NHS report determined that vaping nicotine is “around 95% less harmful than cigarettes,” 62 leading to the development of programs that promote vaping as a tool of risk reduction among current smokers. A 2020 Cochrane review found that vaping nicotine assisted with smoking cessation over placebo 63 and recent work found increased rates of cigarette abstinence (18% v 9.9%) among those switching to vaping compared with conventional nicotine replacement (eg, gum, patch, lozenge). 64 US CDC guidance suggests that vaping nicotine may benefit current adult smokers who are able to achieve complete cigarette cessation by switching to vaping. 65 66
The public health benefit of vaping for smoking cessation is counterbalanced by vaping uptake among never smokers, 2 54 and questions surrounding the safety of chronic vaping. 10 11 Controversy surrounding the NHS claim of vaping as 95% safer than cigarettes has emerged, 67 68 and multiple leading health organizations have concluded that vaping is harmful. 42 69 Studies have demonstrated airborne particulate matter in the proximity of active vapers, 70 and concern remains that secondhand exposure to vaped aerosols may cause adverse effects, complicating the notion of vaping as a net gain for public health. 71 72 Uncertainty about the potential chronic consequences of vaping combined with vaping uptake among never smokers has complicated attempts to generate clear policy guidance. 73 74 Further, many smokers may exhibit “dual use” of conventional cigarettes and vape pens simultaneously, further complicating efforts to understand the impact of vape exposure on respiratory health, and the role vape use may play in smoking cessation. 12 We are unable to know with certainty the extent of nicotine uptake among young people that would have been seen in the absence of vaping availability, and it remains possible that some young vape pen users may have started on conventional cigarettes regardless. That said, declining nicotine use over the past several decades would argue that many young vape pen users would have never had nicotine uptake had vape pens not been introduced. 1 2 It remains an open question whether public health measures encouraging vaping for nicotine cessation will benefit current smokers enough to offset the impact of vaping uptake among young, never smokers. 75
Vaping lung injury—clinical presentations
Vaping related lung injury: 2012-19.
The potential health effects of vape pen use are varied and centered on injury to the airways and lung parenchyma. Before the 2019 EVALI outbreak, the medical literature detailed case reports of sporadic vaping related acute lung injury. The first known case was reported in 2012, when a patient presented with cough, diffuse ground glass opacities, and lipid laden macrophages (LLM) on bronchoalveolar lavage (BAL) return in the context of vape pen use. 76 Over the following seven years, an additional 15 cases of vaping related acute lung injury were reported in the literature. These cases included a wide range of diffuse parenchymal lung disease without any clear unifying features, and included cases of eosinophilic pneumonia, 77 78 79 hypersensitivity pneumonitis, 80 organizing pneumonia, 81 82 diffuse alveolar hemorrhage, 83 84 and giant cell foreign body reaction. 85 Although parenchymal lung injury predominated the cases reported, additional cases detailed episodes of status asthmaticus 86 and pneumothoraces 87 attributed to vaping. Non-respiratory vape pen injury has also been described, including cases of nicotine toxicity from vape solution ingestion, 88 89 and injuries sustained owing to vape pen device explosions. 90
The 2019 EVALI outbreak
In the summer of 2019 the EVALI outbreak led to 2807 cases of idiopathic acute lung injury in predominantly young, healthy individuals, which resulted in 68 deaths. 19 91 Epidemiological work to uncover the cause of the outbreak identified an association with vaping, particularly the use of THC-containing products, among affected individuals. CDC criteria for EVALI ( box 1 ) included individuals presenting with respiratory symptoms who had pulmonary infiltrates on imaging in the context of having vaped or dabbed within 90 days of symptom onset, without an alternative identifiable cause. 92 93 After peaking in September 2019, EVALI case numbers steadily declined, 91 likely owing to identification of a link with vaping, and subsequent removal of offending agents from circulation. Regardless, sporadic cases continue to be reported, and a high index of suspicion is required to differentiate EVALI from covid-19 pneumonia. 94 95 A strong association emerged between EVALI cases and the presence of vitamin E acetate in the BAL return of affected individuals 96 ; however, no definitive causal link has been established. Interestingly, the EVALI outbreak was nearly entirely contained within the US with the exception of several dozen cases, at least one of which was caused by an imported US product. 97 98 99 The pattern of cases and lung injury is most suggestive of a vape solution contaminant that was introduced into the distribution pipeline in US markets, leading to a geographically contained pattern of lung injury among users. CDC case criteria for EVALI may have obscured a potential link between viral pneumonia and EVALI, and cases may have been under-recognized following the onset of the covid-19 pandemic.
CDC criteria for establishing EVALI diagnosis
Cdc lung injury surveillance, primary case definitions, confirmed case.
Vape use* in 90 days prior to symptom onset; and
Pulmonary infiltrate on chest radiograph or ground glass opacities on chest computed tomography (CT) scan; and
Absence of pulmonary infection on initial investigation†; and
Absence of alternative plausible diagnosis (eg, cardiac, rheumatological, or neoplastic process).
Probable case
Pulmonary infiltrate on chest radiograph or ground glass opacities on chest CT; and
Infection has been identified; however is not thought to represent the sole cause of lung injury OR minimum criteria** to exclude infection have not been performed but infection is not thought to be the sole cause of lung injury
*Use of e-cigarette, vape pen, or dabbing.
†Minimum criteria for absence of pulmonary infection: negative respiratory viral panel, negative influenza testing (if supported by local epidemiological data), and all other clinically indicated infectious respiratory disease testing is negative.
EVALI—clinical, radiographic, and pathologic features
In the right clinical context, diagnosis of EVALI includes identification of characteristic radiographic and pathologic features. EVALI patients largely fit a pattern of diffuse, acute lung injury in the context of vape pen exposure. A systematic review of 200 reported cases of EVALI showed that those affected were predominantly men in their teens to early 30s, and most (80%) had been using THC-containing products. 100 Presentations included predominantly respiratory (95%), constitutional (87%), and gastrointestinal symptoms (73%). Radiological studies mostly featured diffuse ground glass opacities bilaterally. Of 92 cases that underwent BAL, alveolar fluid samples were most commonly neutrophil predominant, and 81% were additionally positive for LLM on Oil Red O staining. Lung biopsy was not required to achieve the diagnosis; however, of 33 cases that underwent tissue biopsy, common features included organizing pneumonia, inflammation, foamy macrophages, and fibrinous exudates.
EVALI—outcomes
Most patients with EVALI recovered, and prognosis was generally favorable. A systematic review of identified cases found that most patients with confirmed disease required admission to hospital (94%), and a quarter were intubated. 100 Mortality among EVALI patients was low, with estimates around 2-3% across multiple studies. 101 102 103 Mortality was associated with age over 35 and underlying asthma, cardiac disease, or mental health conditions. 103 Notably, the cohorts studied only included patients who presented for medical care, and the samples are likely biased toward a more symptomatic population. It is likely that many individuals experiencing mild symptoms of EVALI did not present for medical care, and would have self-discontinued vaping following extensive media coverage of the outbreak at that time. Although most EVALI survivors recovered well, case series of some individuals show persistent radiographic abnormalities 101 and sustained reductions in DLCO. 104 105 Pulmonary function evaluation of EVALI survivors showed normalization in FEV 1 /FVC on spirometry in some, 106 while others had more variable outcomes. 105 107 108
Vaping induced lung injury—pathophysiology
The causes underlying vaping related acute lung injury remain interesting to clinicians, scientists, and public health officials; multiple mechanisms of injury have been proposed and are summarized in figure 2 . 31 109 110 Despite increased scientific interest in vaping related lung injury following the EVALI outbreak, the pool of data from which to draw meaningful conclusions is limited because of small scale human studies and ongoing conflicts due to tobacco industry funding. 111 Further, insufficient time has elapsed since widespread vaping uptake, and available studies reflect the effects of vaping on lung health over a maximum 10-15 year timespan. The longitudinal effects of vaping may take decades to fully manifest and ongoing prospective work is required to better understand the impacts of vaping on respiratory health.

Schematic illustrating pathophysiology of vaping lung injury
Pro-inflammatory vape aerosol effects
While multiple pathophysiological pathways have been proposed for vaping related lung injury, they all center on the vape aerosol itself as the conduit of lung inflammation. Vape aerosols have been found to harbor a number of toxic substances, including thermal degradation products of the various vape solution components. 112 Mass spectrometry analysis of vape aerosols has identified a variety of oxidative and pro-inflammatory substances including benzene, acrolein, volatile organic compounds, and propylene oxide. 16 17 Vaping additionally leads to airway deposition of ultrafine particles, 14 113 as well as the heavy metals manganese and zinc which are emitted from the vaping coils. 15 114 Fourth generation vape pens allow for high wattage aerosol generation, which can cause airway epithelial injury and tissue hypoxia, 115 116 as well as formaldehyde exposure similar to that of cigarette smoke. 117 Common carrier solutions such as propylene glycol have been associated with increased airway hyper-reactivity among vape pen users, 31 118 119 and have been associated with chronic respiratory conditions among theater workers exposed to aerosolized propylene glycol used in the generation of artificial fog. 120 Nicotine salts used in pod based vape pen solutions, including Juul, have been found to penetrate the cell membrane and have cytotoxic effects. 121
The myriad available vape pen flavors correlate with an expansive list of chemical compounds with potential adverse respiratory effects. Flavorants have come under increased scrutiny in recent years and have been found to contribute to the majority of aldehyde production during vape aerosol production. 122 Compounds such as cinnamaldehyde, 123 124 2,5-dimethylpyrazine (chocolate flavoring), 125 and 2,3-pentanedione 126 are common flavor additives and have been found to contribute to airway inflammation and altered immunological responses. The flavorant diacetyl garnered particular attention after it was identified on mass spectrometry in most vape solutions tested. 127 Diacetyl is most widely associated with an outbreak of diacetyl associated bronchiolitis obliterans (“popcorn lung”) among workers at a microwave popcorn plant in 2002. 128 Identification of diacetyl in vape solutions raises the possibility of development of a similar pattern of bronchiolitis obliterans among individuals who have chronic vape aerosol exposure to diacetyl-containing vape solutions. 129
Studies of vape aerosols have suggested multiple pro-inflammatory effects on the respiratory system. This includes increased airway resistance, 130 impaired response to infection, 131 and impaired mucociliary clearance. 132 Vape aerosols have further been found to induce oxidative stress in lung epithelial cells, 133 and to both induce DNA damage and impair DNA repair, consistent with a potential carcinogenic effect. 134 Mice chronically exposed to vape aerosols developed increased airway hyper-reactivity and parenchymal changes consistent with chronic obstructive pulmonary disease. 135 Human studies have been more limited, but reveal increased airway edema and friability among vape pen users, as well as altered gene transcription and decreased innate immunity. 136 137 138 Upregulation of neutrophil elastase and matrix metalloproteases among vape users suggests increased proteolysis, potentially putting those patients at risk of chronic respiratory conditions. 139
THC-containing products
Of particular interest during the 2019 EVALI outbreak was the high prevalence of THC use among EVALI cases, 19 raising questions about a novel mechanism of lung injury specific to THC-containing vape solutions. These solutions differ from conventional nicotine based products because of the need for a carrier capable of emulsifying the lipid based THC component. In this context, additional vape solution ingredients rose to attention as potential culprits—namely, THC itself, which has been found to degrade to methacrolein and benzene, 140 as well as vitamin E acetate which was found to be a common oil based diluent. 141
Vitamin E acetate has garnered increasing attention as a potential culprit in the pathophysiology of the EVALI outbreak. Vitamin E acetate was found in 94% of BAL samples collected from EVALI patients, compared with none identified in unaffected vape pen users. 96 Thermal degradation of vitamin E acetate under conditions similar to those in THC vape pens has shown production of ketene, alkene, and benzene, which may mediate epithelial lung injury when inhaled. 39 Previous work had found that vitamin E acetate impairs pulmonary surfactant function, 142 and subsequent studies have shown a dose dependent adverse effect on lung parenchyma by vitamin E acetate, including toxicity to type II pneumocytes, and increased inflammatory cytokines. 143 Mice exposed to aerosols containing vitamin E acetate developed LLM and increased alveolar protein content, suggesting epithelial injury. 140 143
The pathophysiological insult underlying vaping related lung injury may be multitudinous, including potentially compound effects from multiple ingredients comprising a vape aerosol. The heterogeneity of available vape solutions on the market further complicates efforts to pinpoint particular elements of the vape aerosol that may be pathogenic, as no two users are likely to be exposed to the same combination of vape solution products. Further, vape users may be exposed to vape solutions containing terpenes, medium chain triglycerides, or coconut oil, the effects of which on respiratory epithelium remain under investigation. 144
Lipid laden macrophages
Lipid laden alveolar macrophages have risen to prominence as potential markers of vaping related lung injury. Alveolar macrophages describe a scavenger white blood cell responsible for clearing alveolar spaces of particulate matter and modulating the inflammatory response in the lung parenchyma. 145 LLM describe alveolar macrophages that have phagocytosed fat containing deposits, as seen on Oil Red O staining, and have been described in a wide variety of pulmonary conditions, including aspiration, lipoid pneumonia, organizing pneumonia, and medication induced pneumonitis. 146 147 During the EVALI outbreak, LLM were identified in the alveolar spaces of affected patients, both in the BAL fluid and on both transbronchial and surgical lung biopsies. 148 149 Of 52 EVALI cases reported in the literature who underwent BAL, LLM were identified in over 80%. 19 100 101 148 149 150 151 152 153 Accordingly, attention turned to LLM as not only a potential marker of lung injury in EVALI, but as a possible contributor to lung inflammation itself. This concern was compounded by the frequent reported use of oil based THC vape products among EVALI patients, raising the possibility of lipid deposits in the alveolus resulting from inhalation of THC-containing vape aerosols. 154 The combination of LLM, acute lung injury, and inhalational exposure to an oil based substance raised the concern for exogenous lipoid pneumonia. 152 153 However, further evaluation of the radiographic and histopathologic findings failed to identify cardinal features that would support a diagnosis of exogenous lipoid pneumonia—namely, low attenuation areas on CT imaging and foreign body giant cells on histopathology. 155 156 However, differences in the particle size and distribution between vape aerosol exposure and traditional causes of lipoid pneumonia (ie, aspiration of a large volume of an oil-containing substance), could reasonably lead to differences in radiographic appearance, although this would not account for the lack of characteristic histopathologic features on biopsy that would support a diagnosis of lipoid pneumonia.
Recent work suggests that LLM reflect a non-specific marker of vaping, rather than a marker of lung injury. One study found that LLM were not unique to EVALI and could be identified in healthy vape pen users, as well as conventional cigarette smokers, but not in never smokers. 157 Interestingly, this work showed increased cytokines IL-4 and IL-10 among healthy vape users, suggesting that cigarette and vape pen use are associated with a pro-inflammatory state in the lung. 157 An alternative theory supports LLM presence reflecting macrophage clearance of intra-alveolar cell debris rather than exogenous lipid exposure. 149 150 Such a pattern would be in keeping with the role of alveolar macrophages as modulating the inflammatory response in the lung parenchyma. 158 Taken together, available data would support LLM serving as a non-specific marker of vape product use, rather than playing a direct role in vaping related lung injury pathogenesis. 102
Clinical aspects
A high index of suspicion is required in establishing a diagnosis of vaping related lung injury, and a general approach is summarized in figure 3 . Clinicians may consider the diagnosis when faced with a patient with new respiratory symptoms in the context of vape pen use, without an alternative cause to account for their symptoms. Suspicion should be especially high if respiratory complaints are coupled with constitutional and gastrointestinal symptoms. Patients may present with non-specific markers indicative of an ongoing inflammatory process: fevers, leukocytosis, elevated C reactive protein, or elevated erythrocyte sedimentation rate. 19

Flowchart outlining the procedure for diagnosing a vaping related lung injury
Vaping related lung injury is a diagnosis of exclusion. Chest imaging via radiograph or CT may identify a variety of patterns, although diffuse ground glass opacities remain the most common radiographic finding. Generally, patients with an abnormal chest radiograph should undergo a chest CT for further evaluation of possible vaping related lung injury.
Exclusion of infectious causes is recommended. Testing should include evaluation for bacterial and viral causes of pneumonia, as deemed appropriate by clinical judgment and epidemiological data. Exclusion of common viral causes of pneumonia is imperative, particularly influenza and SARS-CoV-2. Bronchoscopy with BAL should be considered on a case-by-case basis for those with more severe disease and may be helpful to identify patients with vaping mediated eosinophilic lung injury. Further, lung biopsy may be beneficial to exclude alternative causes of lung injury in severe cases. 92
No definitive therapy has been identified for the treatment of vaping related lung injury, and data are limited to case reports and public health guidance on the topic. Management includes supportive care and strong consideration for systemic corticosteroids for severe cases of vaping related lung injury. CDC guidance encourages consideration of systemic corticosteroids for patients requiring admission to hospital, or those with higher risk factors for adverse outcomes, including age over 50, immunosuppressed status, or underlying cardiopulmonary disease. 100 Further, given case reports of vaping mediated acute eosinophilic pneumonia, steroids should be implemented in those patients who have undergone a confirmatory BAL. 77 79
Additional therapeutic options include empiric antibiotics and/or antivirals, depending on the clinical scenario. For patients requiring admission to hospital, prompt subspecialty consultation with a pulmonologist can help guide management. Outpatient follow-up with chest imaging and spirometry is recommended, as well as referral to a pulmonologist. Counseling regarding vaping cessation is also a core component in the post-discharge care for this patient population. Interventions specific to vaping cessation remain under investigation; however, literature supports the use of behavioral counseling and/or pharmacotherapy to support nicotine cessation efforts. 66
Health outcomes among vape pen users
Health outcomes among chronic vape pen users remains an open question. To date, no large scale prospective cohort studies exist that can establish a causal link between vape use and adverse respiratory outcomes. One small scale prospective cohort study did not identify any spirometric or radiographic changes among vape pen users over a 3.5 year period. 159 Given that vaping remains a relatively novel phenomenon, many users will have a less than 10 “pack year” history of vape pen use, arguably too brief an exposure period to reflect the potential harmful nature of chronic vaping. Studies encompassing a longer period of observation of vape pen users have not yet taken place, although advances in electronic medical record (EMR) data collection on vaping habits make such work within reach.
Current understanding of the health effects of vaping is largely limited to case reports of acute lung injury, and health surveys drawing associations between vaping exposure and patient reported outcomes. Within these limitations, however, early work suggests a correlation between vape pen use and poorer cardiopulmonary outcomes. Survey studies of teens who regularly vape found increased frequencies of respiratory symptoms, including productive cough, that were independent of smoking status. 160 161 These findings were corroborated in a survey series identifying more severe asthma symptoms and more days of school missed owing to asthma among vape pen users, regardless of cigarette smoking status. 162 163 164 Studies among adults have shown a similar pattern, with increased prevalence of chronic respiratory conditions (ie, asthma or chronic obstructive pulmonary disease) among vape pen users, 165 166 and higher risk of myocardial infarction and stroke, but lower risk of diabetes. 167
The effects of vaping on lung function as determined by spirometric studies are more varied. Reported studies have assessed lung function after a brief exposure to vape aerosols, varying from 5-60 minutes in duration, and no longer term observational cohort studies exist. While some studies have shown increased airway resistance after vaping exposure, 130 168 169 others have shown no change in lung function. 137 170 171 The cumulative exposure of habitual vape pen users to vape aerosols is much longer than the period evaluated in these studies, and the impact of vaping on longer term respiratory heath remains to be seen. Recent work evaluating ventilation-perfusion matching among chronic vapers compared with healthy controls found increased ventilation-perfusion mismatch, despite normal spirometry in both groups. 172 Such work reinforces the notion that changes in spirometry are a feature of more advanced airways disease, and early studies, although inconsistent, may foreshadow future respiratory impairment in chronic vapers.
Covid-19 and vaping
The covid-19 pandemic brought renewed attention to the potential health impacts of vaping. Studies investigating the role of vaping in covid-19 prevalence and outcomes have been limited by the small size of the populations studied and results have been inconsistent. Early work noted a geographic association in the US between vaping prevalence and covid-19 cases, 173 and a subsequent survey study found that a covid-19 diagnosis was five times more likely among teens who had ever vaped. 174 In contrast, a UK survey study found no association between vaping status and covid-19 infection rates, although captured a much smaller population of vape pen users. 175 Reports of nicotine use upregulating the angiotensin converting enzyme 2 (ACE-2) receptor, 176 which serves as the binding site for SARS-CoV-2 entry, raised the possibility of increased susceptibility to covid-19 among chronic nicotine vape pen users. 177 178 Further, vape use associated with sharing devices and frequent touching of the mouth and face were posited as potential confounders contributing to increased prevalence of covid-19 in this population. 179
Covid-19 outcomes among chronic vape pen users remain an open question. While smoking has been associated with progression to more severe infections, 180 181 no investigation has been performed to date among vaping cohorts. The young average age of chronic vape pen users may prove a protective factor, as risk of severe covid-19 infection has been shown to increase with age. 182 Regardless, a prudent recommendation remains to abstain from vaping to mitigate risk of progression to severe covid-19 infection. 183
Increased awareness of respiratory health brought about by covid-19 and EVALI is galvanizing the changing patterns in vape pen use. 184 Survey studies have consistently shown trends toward decreasing use among adolescents and young adults. 174 185 186 In one study, up to two thirds of participants endorsed decreasing or quitting vaping owing to a combination of factors including difficulty purchasing vape products during the pandemic, concerns about vaping effects on lung health, and difficulty concealing vape use while living with family. 174 Such results are reflected in nationwide trends that show halting growth in vaping use among high school students. 8 These trends are encouraging in that public health interventions countering nicotine use among teens may be meeting some measure of success.
Clinical impact—collecting and recording a vaping history
Vaping history in electronic medical records.
Efforts to prevent, diagnose, and treat vaping related lung injury begin with the ability of our healthcare system to identify vape users. Since vaping related lung injury remains a diagnosis of exclusion, clinicians must have a high index of suspicion when confronted with idiopathic lung injury in a patient with vaping exposure. Unlike cigarette use, vape pen use is not built into most EMR systems, and is not included in meaningful use criteria for EMRs. 187 Retrospective analysis of outpatient visits showed that a vaping history was collected in less than 0.1% of patients in 2015, 188 although this number has been increasing. 189 190 In part augmented by EMR frameworks that prompt collection of data on vaping history, more recent estimates indicate that a vaping history is being collected in up to 6% of patients. 191 Compared with the widespread use of vaping, particularly among adolescent and young adult populations, this number remains low. Considering generational trends in nicotine use, vaping will likely eventually overcome cigarettes as the most common mode of nicotine use, raising the importance of collecting a vaping related history. Further, EMR integration of vaping history is imperative to allow for retrospective, large scale analyses of vape exposure on longitudinal health outcomes at a population level.
Practical considerations—gathering a vaping history
As vaping becomes more common, the clinician’s ability to accurately collect a vaping history and identify patients who may benefit from nicotine cessation programs becomes more important. Reassuringly, gathering a vaping history is not dissimilar to asking about smoking and use of other tobacco products, and is summarized in box 2 . Collecting a vaping history is of particular importance for providers caring for adolescents and young adults who are among the highest risk demographics for vape pen use. Adolescents and young adults may be reluctant to share their vaping history, particularly if they are using THC-containing or CBD-containing vape solutions. Familiarity with vernacular terms to describe vaping, assuming a non-judgmental approach, and asking parents or guardians to step away during history taking will help to break down these barriers. 192
Practical guide to collecting a vaping history
Ask with empathy.
Young adults may be reluctant to share history of vaping use. Familiarity with vaping terminology, asking in a non-judgmental manner, and asking in a confidential space may help.
Ask what they are vaping
Vape products— vape pens commonly contain nicotine or an alternative active ingredient, such as THC or CBD. Providers may also inquire about flavorants, or other vape solution additives, that their patient is consuming, particularly if vaping related lung injury is suspected.
Source— ask where they source their product from. Sources may include commercially available products, third party distributors, or friends or local contacts.
Ask how they are vaping
Device— What style of device are they using?
Frequency— How many times a day do they use their vape pen (with frequent use considered >5 times a day)? Alternatively, providers may inquire how long it takes to deplete a vape solution cartridge (with use of one or more pods a day considered heavy use).
Nicotine concentration— For individuals consuming nicotine-containing products, clinicians may inquire about concentration and frequency of use, as this may allow for development of a nicotine replacement therapy plan.

Ask about other inhaled products
Clinicians should ask patients who vape about use of other inhaled products, particularly cigarettes. Further, clinicians may ask about use of water pipes, heat-not-burn devices, THC-containing products, or dabbing.
The following provides a practical guide on considerations when collecting a vaping history. Of note, collecting a partial history is preferable to no history at all, and simply recording whether a patient is vaping or not adds valuable information to the medical record.
Vape use— age at time of vaping onset and frequency of vape pen use. Vape pen use >5 times a day would be considered frequent. Alternatively, clinicians may inquire how long it takes to deplete a vape solution pod (use of one or more pods a day would be considered heavy use), or how frequently users are refilling their vape pens for refillable models.
Vape products— given significant variation in vape solutions available on the market, and variable risk profiles of the multitude of additives, inquiring as to which products a patient is using may add useful information. Further, clinicians may inquire about use of nicotine versus THC-containing vape solutions, and whether said products are commercially available or are customized by third party sellers.
Concurrent smoking— simultaneous use of multiple inhaled products is common among vape users, including concurrent use of conventional cigarettes, water pipes, heat-not-burn devices, and THC-containing or CBD-containing products. Among those using marijuana products, gathering a history regarding the type of product use, the device, and the modality of aerosol generation may be warranted. Gathering such detailed information may be challenging in the face of rapidly evolving product availability and changing popular terminology. Lastly, clinicians may wish to inquire about “dabbing”—the practice of inhaling heated butane hash oil, a concentrated THC wax—which may also be associated with lung injury. 193
Future directions
Our understanding of the effects of vaping on respiratory health is in its early stages and multiple trials are under way. Future work requires enhanced understanding of the effects of vape aerosols on lung biology, such as ongoing investigations into biomarkers of oxidative stress and inflammation among vape users (clinicaltrials.gov NCT03823885 ). Additional studies seek to elucidate the relation between vape aerosol exposure and cardiopulmonary outcomes among vape pen users ( NCT03863509 , NCT05199480 ), while an ongoing prospective cohort study will allow for longitudinal assessment of airway reactivity and spirometric changes among chronic vape pen users ( NCT04395274 ).
Public health and policy interventions are vital in supporting both our understanding of vaping on respiratory health and curbing the vaping epidemic among teens. Ongoing, large scale randomized controlled studies seek to assess the impact of the FDA’s “The Real Cost” advertisement campaign for vaping prevention ( NCT04836455 ) and another trial is assessing the impact of a vaping prevention curriculum among adolescents ( NCT04843501 ). Current trials are seeking to understand the potential for various therapies as tools for vaping cessation, including nicotine patches ( NCT04974580 ), varenicline ( NCT04602494 ), and text message intervention ( NCT04919590 ).
Finally, evaluation of vaping as a potential tool for harm reduction among current cigarette smokers is undergoing further evaluation ( NCT03235505 ), which will add to the body of work and eventually lead to clear policy guidance.
Several guidelines on the management of vaping related lung injury have been published and are summarized in table 1 . 194 195 196 Given the relatively small number of cases, the fact that vaping related lung injury remains a newer clinical entity, and the lack of clinical trials on the topic, guideline recommendations reflect best practices and expert opinion. Further, published guidelines focus on the diagnosis and management of EVALI, and no guidelines exist to date for the management of vaping related lung injury more generally.
Summary of clinical guidelines
- View inline
Conclusions
Vaping has grown in popularity internationally over the past decade, in part propelled by innovations in vape pen design and nicotine flavoring. Teens and young adults have seen the biggest uptake in use of vape pens, which have superseded conventional cigarettes as the preferred modality of nicotine consumption. Despite their widespread popularity, relatively little is known about the potential effects of chronic vaping on the respiratory system, and a growing body of literature supports the notion that vaping is not without risk. The 2019 EVALI outbreak highlighted the potential harms of vaping, and the consequences of long term use remain unknown.
Discussions regarding the potential harms of vaping are reminiscent of scientific debates about the health effects of cigarette use in the 1940s. Interesting parallels persist, including the fact that only a minority of conventional cigarette users develop acute lung injury, yet the health impact of sustained, longitudinal cigarette use is unquestioned. The true impact of vaping on respiratory health will manifest over the coming decades, but in the interval a prudent and time tested recommendation remains to abstain from consumption of inhaled nicotine and other products.
Questions for future research
How does chronic vape aerosol exposure affect respiratory health?
Does use of vape pens affect respiratory physiology (airway resistance, V/Q matching, etc) in those with underlying lung disease?
What is the role for vape pen use in promoting smoking cessation?
What is the significance of pulmonary alveolar macrophages in the pathophysiology of vaping related lung injury?
Are particular populations more susceptible to vaping related lung injury (ie, by sex, demographic, underlying comorbidity, or age)?
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: AJ conceived of, researched, and wrote the piece. She is the guarantor.
Competing interests: I have read and understood the BMJ policy on declaration of interests and declare the following interests: AJ receives consulting fees from DawnLight, Inc for work unrelated to this piece.
Patient involvement: No patients were directly involved in the creation of this article.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ US Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the Surgeon General. 2014. doi: 10.1037/e510072014-001 .
- Cornelius ME ,
- Loretan CG ,
- Marshall TR
- Fetterman JL ,
- Benjamin EJ ,
- Barrington-Trimis JL ,
- Leventhal AM ,
- Cullen KA ,
- Gentzke AS ,
- Sawdey MD ,
- ↵ Centers for Disease Control and Prevention. Surgeon General’s Advisory on E-cigarette Use Among Youth. 2018. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/surgeon-general-advisory/index.html
- Leventhal A ,
- Johnston L ,
- O’Malley PM ,
- Patrick ME ,
- Barrington-Trimis J
- ↵ Foundation for a Smoke-Free World https://www.smokefreeworld.org/published_reports/
- Kaisar MA ,
- Calfee CS ,
- Matthay MA ,
- ↵ Royal College of Physicians (London) & Tobacco Advisory Group. Nicotine without smoke: tobacco harm reduction: a report. 2016. https://www.rcplondon.ac.uk/projects/outputs/nicotine-without-smoke-tobacco-harm-reduction
- ↵ National Academies of Sciences, Engineering, and Medicine. Public health consequences of e-cigarettes. 2018. doi: 10.17226/24952 OpenUrl CrossRef
- Manigrasso M ,
- Buonanno G ,
- Stabile L ,
- Agnihotri R
- LeBouf RF ,
- Koutrakis P ,
- Christiani DC
- Perrine CG ,
- Pickens CM ,
- Boehmer TK ,
- Lung Injury Response Epidemiology/Surveillance Group
- Layden JE ,
- Esposito S ,
- Spindle TR ,
- Eissenberg T ,
- Kendler KS ,
- McCabe SE ,
- ↵ Joseph R. Electric vaporizer. 1930.
- ↵ Gilbert HA. Smokeless non-tobacco cigarette. 1965.
- ↵ An Interview With A 1970’s Vaping Pioneer. Ashtray Blog. 2015 . https://www.ecigarettedirect.co.uk/ashtray-blog/2014/06/favor-cigarette-interview-dr-norman-jacobson.html (2014).
- Benowitz N ,
- ↵ National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, & Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems. Public Health Consequences of E-Cigarettes . (National Academies Press (US), 2018).
- ↵ Tolentino J. The Promise of Vaping and the Rise of Juul. The New Yorker . 2018 https://www.newyorker.com/magazine/2018/05/14/the-promise-of-vaping-and-the-rise-of-juul
- ↵ Bowen A, Xing C. Nicotine salt formulations for aerosol devices and methods thereof. 2014.
- Madden DR ,
- McConnell R ,
- Gammon DG ,
- Marynak KL ,
- ↵ Jackler RK, Chau C, Getachew BD, et al. JUUL Advertising Over its First Three Years on the Market. Stanford Research into the Impact of Tobacco Advertising, Stanford University School of Medicine. 2019. https://tobacco-img.stanford.edu/wp-content/uploads/2021/07/21231836/JUUL_Marketing_Stanford.pdf
- Prochaska JJ ,
- ↵ Richtel M, Kaplan S. Juul May Get Billions in Deal With One of World’s Largest Tobacco Companies. The New York Times . 2018.
- ↵ Truth Initiative. Vaping Lingo Dictionary: A guide to popular terms and devices. 2020. https://truthinitiative.org/research-resources/emerging-tobacco-products/vaping-lingo-dictionary
- Williams M ,
- Pepper JK ,
- MacMonegle AJ ,
- Nonnemaker JM
- ↵ The Physics of Vaporization. Jupiter Research. 2020. https://www.jupiterresearch.com/physics-of-vaporization/
- Bonnevie E ,
- ↵ National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. 2016. https://www.ncbi.nlm.nih.gov/books/NBK538680/
- Trivers KF ,
- Phillips E ,
- Stefanac S ,
- Sandner I ,
- Grabovac I ,
- ↵ Knowledge-Action-Change. Burning Issues: The Global State of Tobacco Harm Reduction 2020. 2020. https://gsthr.org/resources/item/burning-issues-global-state-tobacco-harm-reduction-2020
- Creamer MR ,
- Park-Lee E ,
- Gorukanti A ,
- Delucchi K ,
- Fisher-Travis R ,
- Halpern-Felsher B
- Amrock SM ,
- ↵ Buy JUUL Products | Shop All JUULpods, JUUL Devices, and Accessories | JUUL. https://www.juul.com/shop
- Schiff SJ ,
- Kechter A ,
- Simpson KA ,
- Ceasar RC ,
- Braymiller JL ,
- Barrington-Trimis JL
- Moustafa AF ,
- Rodriguez D ,
- Audrain-McGovern J
- Berhane K ,
- Stjepanović D ,
- Hitchman SC ,
- Bakolis I ,
- Plurphanswat N
- Warner KE ,
- Cummings KM ,
- ↵ FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint. FDA . 2020 . https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children
- ↵ Henderson, E. E-cigarettes: an evidence update. 113.
- Hartmann-Boyce J ,
- McRobbie H ,
- Lindson N ,
- Phillips-Waller A ,
- ↵ Centers for Disease Control and Prevention. Electronic Cigarettes. 2020. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/index.htm l
- Patnode CD ,
- Henderson JT ,
- Thompson JH ,
- Senger CA ,
- Fortmann SP ,
- Whitlock EP
- Kmietowicz Z
- ↵ World Health Organization. E-cigarettes are harmful to health. 2020. https://www.who.int/news/item/05-02-2020-e-cigarettes-are-harmful-to-health
- Lachireddy K ,
- Sleiman M ,
- Montesinos VN ,
- Kalkhoran S ,
- Filion KB ,
- Kimmelman J ,
- Eisenberg MJ
- McCauley L ,
- Aoshiba K ,
- Nakamura H ,
- Wiggins A ,
- Hudspath C ,
- Kisling A ,
- Hostler DC ,
- Sommerfeld CG ,
- Weiner DJ ,
- Mantilla RD ,
- Darnell RT ,
- Khateeb F ,
- Agustin M ,
- Yamamoto M ,
- Cabrera F ,
- ↵ Long. Diffuse Alveolar Hemorrhage Due to Electronic Cigarette Use | A54. CRITICAL CARE CASE REPORTS: ACUTE HYPOXEMIC RESPIRATORY FAILURE/ARDS. https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2016.193.1_MeetingAbstracts.A1862
- Ring Madsen L ,
- Vinther Krarup NH ,
- Bergmann TK ,
- Bradford LE ,
- Rebuli ME ,
- Jaspers I ,
- Clement KC ,
- Loughlin CE
- Bonilla A ,
- Alamro SM ,
- Bassett RA ,
- Osterhoudt K ,
- Slaughter J ,
- ↵ Health CO. on S. and. Smoking and Tobacco Use; Electronic Cigarettes. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html (2019).
- ↵ For State, Local, Territorial, and Tribal Health Departments | Electronic Cigarettes | Smoking & Tobacco Use | CDC. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease/health-departments/index.html (2019).
- ↵ 2019 Lung Injury Surveillance Primary Case Definitions. 2.
- Callahan SJ ,
- Collingridge DS ,
- Armatas C ,
- Heinzerling A ,
- Blount BC ,
- Karwowski MP ,
- Shields PG ,
- Lung Injury Response Laboratory Working Group
- ↵ Government of Canada. Vaping-associated lung illness. 2020. https://www.canada.ca/en/public-health/services/diseases/vaping-pulmonary-illness.html (2020).
- Marlière C ,
- De Greef J ,
- Casanova GS ,
- Blagev DP ,
- Guidry DW ,
- Grissom CK ,
- Werner AK ,
- Koumans EH ,
- Chatham-Stephens K ,
- Lung Injury Response Mortality Working Group
- Tsirilakis K ,
- Yenduri NJS ,
- Guillerman RP ,
- Anderson B ,
- Serajeddini H ,
- Knipping D ,
- Brasky TM ,
- Pisinger C ,
- Godtfredsen N ,
- Jensen RP ,
- Pankow JF ,
- Strongin RM ,
- Lechasseur A ,
- Altmejd S ,
- Turgeon N ,
- Goessler W ,
- Chaumont M ,
- van de Borne P ,
- Bernard A ,
- Kosmider L ,
- Sobczak A ,
- Aldridge K ,
- Afshar-Mohajer N ,
- Koehler K ,
- Varughese S ,
- Teschke K ,
- van Netten C ,
- Beyazcicek O ,
- Onyenwoke RU ,
- Khlystov A ,
- Samburova V
- Lavrich KS ,
- van Heusden CA ,
- Lazarowski ER ,
- Carson JL ,
- Pawlak EA ,
- Lackey JT ,
- Sherwood CL ,
- O’Sullivan M ,
- Vallarino J ,
- Flanigan SS ,
- LeBlanc M ,
- Kullman G ,
- Simoes EJ ,
- Wambui DW ,
- Vardavas CI ,
- Anagnostopoulos N ,
- Kougias M ,
- Evangelopoulou V ,
- Connolly GN ,
- Behrakis PK
- Sussan TE ,
- Gajghate S ,
- Thimmulappa RK ,
- Hossain E ,
- Perveen Z ,
- Lerner CA ,
- Sundar IK ,
- Garcia-Arcos I ,
- Geraghty P ,
- Baumlin N ,
- Coakley RC ,
- Mascenik T ,
- Staudt MR ,
- Hollmann C ,
- Radicioni G ,
- Coakley RD ,
- Kalathil SG ,
- Bogner PN ,
- Goniewicz ML ,
- Thanavala YM
- Massey JB ,
- Matsumoto S ,
- Traber MG ,
- Ranpara A ,
- Stefaniak AB ,
- Williams K ,
- Fernandez E ,
- Basset-Léobon C ,
- Lacoste-Collin L ,
- Courtade-Saïdi M
- Boland JM ,
- Maddock SD ,
- Cirulis MM ,
- Tazelaar HD ,
- Mukhopadhyay S ,
- Dammert P ,
- Kalininskiy A ,
- Davidson K ,
- Brancato A ,
- Heetderks P ,
- Dicpinigaitis PV ,
- Trachuk P ,
- Suhrland MJ
- Khilnani GC
- Simmons A ,
- Freudenheim JL ,
- Hussell T ,
- Cibella F ,
- Caponnetto P ,
- Schweitzer RJ ,
- Williams RJ ,
- Vindhyal MR ,
- Munguti C ,
- Vindhyal S ,
- Lappas AS ,
- Tzortzi AS ,
- Konstantinidi EM ,
- Antoniewicz L ,
- Brynedal A ,
- Lundbäck M ,
- Ferrari M ,
- Boulay MÈ ,
- Boulet LP ,
- Morissette MC
- Kizhakke Puliyakote AS ,
- Elliott AR ,
- Anderson KM ,
- Crotty Alexander LE ,
- Jackson SE ,
- McAlinden KD ,
- McKelvey K ,
- Patanavanich R ,
- NVSS - Provisional Death Counts for COVID-19 - Executive Summary
- Sokolovsky AW ,
- Hertel AW ,
- Micalizzi L ,
- Klemperer EM ,
- Peasley-Miklus C ,
- Villanti AC
- Henricks WH
- Young-Wolff KC ,
- Klebaner D ,
- Mowery DL ,
- Don’t Forget to Ask
- Stephens D ,
- Siegel DA ,
- Jatlaoui TC ,
- Lung Injury Response Clinical Working Group ,
- Ramalingam SS ,
- Schuurmans MM
Vaping – Top 3 Pros and Cons
Vaping is the act of using e-cigarettes, which were first introduced in the United States around 2006. [ 5 ]
E-cigarettes are battery-powered devices that heat a liquid into an aerosol vapor for inhalation. The liquid used in e-cigarettes is also known as e-liquid or vape juice. The main components are generally flavoring, nicotine, and water, along with vegetable glycerin and propylene glycol, which distribute the flavor and nicotine in the liquid and create the vapor. Popular flavorings include mint, mango, and tobacco. [ 3 ] [ 4 ] [ 44 ] [ 45 ]
E-cigarettes are also known as “e-cigs,” “e-hookahs,” “mods,” “vape pens,” “vapes,” “vaporizers,” “e-pipes,” and “electronic nicotine delivery systems (ENDS).” Some e-cigarettes are made to resemble regular cigarettes, cigars, or pipes, while others look like pens or USB flash drives. [ 7 ] [ 42 ] [ 43 ]
The JUUL brand of e-cigarettes, a vaporizer shaped like a USB drive, launched in 2015 and captured nearly 75% of the market in 2018, becoming so popular that vaping is often referred to as “juuling.” Juul’s market popularity has since declined to 42% in 2020. [ 7 ] [ 8 ] [ 9 ] [ 51 ]
The US Food and Drug Administration (FDA) has regulated e-cigarettes as a tobacco product since 2016. On Sep. 11, 2019, the Trump administration announced plans to have the FDA end sales of non-tobacco e-cigarette flavors such as mint or menthol in response to concerns over teen vaping. E-cigarette manufacturers were required to request FDA permission to keep flavored products on the market. The FDA had until Sep. 9, 2021 to make a decision. [ 6 ][ 46 ] [ 49 ]
On Sep. 9, 2021, Acting FDA Commissioner Janet Woodcock and Director of the FDA’s Center for Tobacco Products Mitch Zeller announced that the FDA had made decisions on 93% of the 6.5 million submitted applications for “deemed” new tobacco products (“‘deemed’ new” means the FDA newly has authority to review the products but the products may already be on the market), including denying 946,000 vaping products “because their applications lacked sufficient evidence that they have a benefit to adult smokers to overcome the public health threat posed by the well-documented, alarming levels of youth use.” The FDA had taken no action on JUUL products as of Sep. 9. [ 55 ] [ 56 ] [ 57 ]
On Oct. 12, 2021, the FDA authorized the Vuse e-cigarette and cartridges, marketed by R.J. Reynolds one of the world’s largest cigarette manufacturers. The move is the first time the FDA authorized any vaping product. According to a statement from the FDA, the organization “determined that the potential benefit to smokers who switch completely or significantly reduce their cigarette use, would outweigh the risk to youth.” [ 58 ]
On June 23, 2022, the FDA ordered Juul to stop selling “all of their products currently marketed in the United States.” The order included removing products currently on the market, including Juul devices (vape pens) and pods (cartridges). The following day, June 24, 2022, a federal appeals court temporarily put the ban on hold while the court reviewed Juul’s appeal. On Sep. 6, 2022, Juul settled a lawsuit brought by almost 36 states and Puerto Rico. The states and Puerto Rico accused Juul of marketing to minors. Juul admitted no wrongdoing in settling the lawsuit, but the company will have to pay $438.5 million, stop marketing to youth, stop funding education in schools, and stop misrepresenting the amount of nicotine in the products. [ 61 ] [ 62 ] [ 63 ]
On June, 21, 2024, the FDA approved four types of menthol-flavored vapes made by NJOY. The approval makes the vapes the first flavored e-cigarettes that can be legally sold in the United States. The move comes amid a debate about whether to ban traditional menthol cigarettes at the federal level. [ 64 ]
Nearly 11 million American adults used e-cigarettes in 2018, more than half of whom were under age 35. One in five high school students used e-cigarettes to vape nicotine in 2018. E-cigarettes were the fourth most popular tobacco products with 4% of retail sales, behind traditional cigarettes (83%), chewing/smokeless tobacco (8%), and cigars (5%) as of Feb. 2019. The global e-cigarette and vape market was worth $15.04 billion in 2020. [ 1 ][ 2 ][ 8 ] [ 50 ]
According to the most recent CDC data (2018), 9.7% of current cigarette smokers were also current vapers, though 49.4% of current smokers had vaped at some point. Of former smokers who had quit within the last year, 25.2% were current vapers and 57.3% had tried vaping. Of former smokers who quit one to four years ago, 17.3% were current vapers and and 48.6% had tried vaping. Of former smokers who quit five or more years ago, 1.7% were current vapers and 9% had tried vaping. And of people who have never smoked, 1.5% were current vapers and 6.5% had tried vaping. [ 52 ]
18-29 year olds were more likely to say they vaped (17%) than smoked cigarettes, while every older age group was more likely to smoke than vape. [ 54 ]
Is Vaping with E-Cigarettes Safe?
Pro 1 E-cigarettes help adults quit smoking and lowers youth smoking rates. A July 2019 study found that cigarettes smokers who picked up vaping were 67% more likely to quit smoking. A New England Journal of Medicine study found that e-cigarettes are twice as effective at getting people to quit smoking as traditional nicotine replacements such as the patch and gum. E-cigarettes caused a 50% increase in the rate of people using a product designed to help people quit smoking. [ 14 ] [ 15 ] [ 48 ] Peter Hajek, Professor of Clinical Psychology at Queen Mary University London, said, “smokers who switch to vaping remove almost all the risks smoking poses to their health.” [ 13 ] Vaping has likely contributed to record low levels of youth cigarette smoking, which hit a record-low of just 4.6% of high school students in 2020, down from 19.8% in 2006 (the year e-cigarettes were introduced in the United States). [ 19 ] [ 20 ] [ 53 ] Further, a report from Public Health England found no evidence that vaping is an entry into smoking for young people. [ 21 ] Read More
Pro 2 Vaping is a safer way to ingest tobacco. A UK government report stated that the “best estimates show e-cigarettes are 95% less harmful to your health than normal cigarettes.” [ 16 ] Matthew Carpenter, Co-Director of the Tobacco Research Program at the Hollings Cancer Center, said, “Combustible cigarettes are the most harmful form of nicotine delivery.” [ 17 ] E-cigarettes are safer for indoor use. Researchers found that the level of nicotine on surfaces in the homes of e-cigarette users was nearly 200 times lower than in the homes of traditional cigarette smokers. Nicotine left behind on surfaces can turn into carcinogens; the amount of nicotine found where vapers live was similar to the trace amounts in the homes of nonsmokers. [ 1 ] [ 18 ] Traditional cigarettes are known to cause health problems such as lung cancer, heart disease, and stroke. Worldwide, smoking is the top cause of preventable death, responsible for over seven million deaths each year. [ 10 ] The National Academies of Science, Engineering, and Medicine found conclusive evidence that switching to e-cigarettes reduces exposure to toxicants and carcinogens. Burning a traditional cigarette releases noxious gases such as carbon monoxide. Cigarette smoke contains tar, which accounts for most of the carcinogens associated with smoking. E-cigarettes don’t have those gases or tar. [ 11 ] [ 12 ] Read More
Pro 3 E-cigarettes reduce health care costs, create jobs, and help the economy. Sally Satel, a psychiatrist specializing in addiction and resident scholar at the American Enterprise Institute, argued, “promoting electronic cigarettes to smokers should be a public health priority. Given that the direct medical costs of smoking are estimated to be more than $130 billion per year, along with $150 billion annually in productivity losses from premature deaths, getting more smokers to switch would result in significant cost savings — as well as almost half a million lives saved each year.” [ 22 ] Grover Norquist and Paul Blair, both of Americans for Tax Reform, stated, “e-cigarettes and vapor products are the Uber of the product industry. They’re a disruptive and innovative technology… Thousands of good-paying jobs are being created by an industry that is probably going to save hundreds of thousands of lives.” [ 23 ] Tax policy economist J. Scott Moody calculated that the harm reduction from smokers switching to vaping could save $48 billion in annual Medicaid spending. [ 24 ] Juul created more than 1,200 jobs just in 2018. A letter signed by a coalition of anti-regulation groups warned that efforts to limit the e-cigarette industry would destroy tens of thousands of jobs for manufacturers of the devices and the stores that sell them. [ 7 ] [ 25 ] Read More
Con 1 Vaping among kids is skyrocketing: addicting a new generation to nicotine and introducing them to smoking. An Oct. 25, 2021 study found marijuana vaping by teens doubled between 2013 and 2020, and the number of minors who stated they’d vaped marijuana in the past 30 days rose from 1.6% to 8.4% in the same time. [ 59 ] US Surgeon General Jerome Adams declared youth e-cigarette use an “epidemic,” noting a 900% increase in vaping by middle and high school students between 2011 and 2015. [ 2 ] As of 2020, 19.6% of high school students used e-cigarettes, the most-used tobacco product among the age group, followed by cigars (5%). Teens who use e-cigarettes are four times more likely to try regular cigarettes than their peers who never used tobacco, and 21.8% of youth cigarette use may be attributable to initiation through vaping. [ 26 ] [ 53 ] Nancy Brown, CEO of the American Heart Association, stated, “The tobacco industry is well aware that flavored tobacco products [such as e-cigarettes] appeal to youth and has taken advantage of this by marketing them in a wide range of fruit and candy flavors.” [ 30 ] Read More
Con 2 Vaping causes serious health risks, including depression, lung disease, and stroke. Nicotine use by young people may increase the risk of addiction to other drugs and impair prefrontal brain development, which can lead to ADD and disrupt impulse control. Adult vapers are also more than twice as likely to be diagnosed as depressed than their non-vaping peers. [ 12 ] [ 27 ] [ 28 ] [ 29 ] [ 60 ] The CDC confirmed six vaping-related deaths and over 450 possible cases of lung illness associated with e-cigarettes as of Sep. 6, 2019. People who use e-cigarettes have a 71% increased risk of stroke and 40% higher risk of heart disease, as compared to nonusers. Studies have shown that e-cigarettes can cause arterial stiffness and cardiovascular harm, and may increase the odds of a heart attack by 42%. [ 31 ] [ 32 ] [ 33 ] [ 47 ] Researchers who found increased risk of blood clots from e-cigarettes wrote, “these devices do emit considerable levels of toxicants, some of which are shared/overlap with tobacco smoking; and thus their harm should not be underestimated.” [ 33 ] Scientists at Johns Hopkins Bloomberg School of Public Health found that e-cigarettes leak toxic metals, possibly from the heating coils, that are associated with health problems such as kidney disease, respiratory irritation, shortness of breath, and more. [ 34 ] Some ingredients in the liquids used in e-cigarettes change composition when they are heated, leading to inhalation of harmful compounds such as formaldehyde, which is carcinogenic. [ 35 ] Read More
Con 3 E-cigarettes can catch fire and even explode. E-cigarette explosions have led to the loss of body parts (such as an eye, tongue, or tooth), third degree burns, holes in the roof of the mouth, and death. [ 36 ] Researchers at George Mason University found that 2,035 people sought emergency room treatment for burn or explosion injuries from e-cigarettes between 2015 and 2017, and believe there were more injuries that went untreated. They also found more than 40 times the number of injuries reported by the FDA between 2009 and 2015. [ 36 ] [ 37 ] Airlines prohibit e-cigarettes in checked baggage due to the possibility of their lithium batteries catching fire. In Jan. 2019, a passenger’s e-cigarette overheated and caught fire in the airplane cabin. That same month, a Texas man died when debris from an e-cigarette explosion tore his carotid artery. In 2018, a man in Florida was killed by shrapnel from his e-cigarette exploding. [ 38 ] [ 39 ] [ 40 ] The US Fire Administration (USFA) found 195 reports of e-cigarette explosions and fires including 133 acute injuries, of which 29% were severe. The USFA stated, “No other consumer product that is typically used so close to the human body contains the lithium-ion battery that is the root cause of the incidents.” [ 41 ] Read More

Discussion Questions
1. Is vaping safe? Explain your answer.
2. Should vaping restrictions or prohibitions be placed on teens? Why or why not?
3. While this article focuses on nicotine e-cigarettes, consider the safety of marijuana vaping.
Take Action
1. Consider Consumer Advocates for Smoke-free Alternatives Association’s take on vaping as a cigarette alternative
2. Learn about e-cigarettes at Encyclopaedia Britannica.
3. Analyze the science of vaping at the American Heart Association .
4. Consider how you felt about the issue before reading this article. After reading the pros and cons on this topic, has your thinking changed? If so, how? List two to three ways. If your thoughts have not changed, list two to three ways your better understanding of the “other side of the issue” now helps you better argue your position.
5. Push for the position and policies you support by writing US national senators and representatives .
| 1. | Lisa Rapaport, “Almost One in 20 U.S. Adults Now Use E-Cigarettes,” reuters.com, Aug. 27, 2018 | |
| 2. | Jerome Adams, “Surgeon General’s Advisory on E-cigarette Use Among Youth,” e-cigarettes.surgeongeneral.gov, Jan. 10, 2019 | |
| 3. | National Institute on Drug Abuse, “Electronic Cigarettes (E-cigarettes),” drugabuse.gov, June 2018 | |
| 4. | Lori Higgins, “Your Kids Think It’s Cool to Vape at School. It’s a Big Problem.,” freep.com, Sep. 25, 2018 | |
| 5. | NBC News, “Vaping 101: How Do E-Cigarettes Work?,” nbcnews.com, Apr. 24, 2014 | |
| 6. | FDA, “The Facts on the FDA’s New Tobacco Rule,” fda.gov, Nov. 9, 2017 | |
| 7. | Richard Craver, “FDA Scrutiny of Juul Not Affecting Dominant Market Share,” journalnow.com, Jan. 23, 2019 | |
| 8. | Richard Craver, “Juul Market Share Slips following Removal of Fruity-flavored E-cigs,” journalnow.com, Feb. 5, 2019 | |
| 9. | Angelica LaVito, “Fda Chief Accuses Juul, Altria of Reneging on Promise to Combat ‘Epidemic’ Teen Vaping Use,” usatoday.com, Feb. 8, 2019 | |
| 10. | CDC, “Smoking & Tobacco Use,” cdc.gov, Feb. 6, 2019 | |
| 11. | National Academies of Science, Engineering, and Medicine, “Public Health Consequences of E-Cigarettes,” nap.edu, 2018 | |
| 12. | John Ross, “E-Cigarettes: Good News, Bad News,” health.harvard.edu, July 25, 2016 | |
| 13. | James Meikle, “Vaping: E-Cigarettes Safer Than Smoking, Says Public Health England,” theguardian.com, Aug. 19, 2015 | |
| 14. | Peter Hajek, Anna Phillips-Waller, Dunja Przulj, et al., “A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy,” New England Journal of Medicine, Jan. 30, 2019 | |
| 15. | Yue-Lin Zhuang, Sharon E. Cummins, Jessica Y. Sun, and Shu-Hong Zhu, “Long-Term E-Cigarette Use and Smoking Cessation: A Longitudinal Study with US Population,” Tobacco Control, 2016 | |
| 16. | Public Health England, “E-Cigarettes Around 95% Less Harmful Than Tobacco Estimates Landmark Review,” gov.uk, Aug. 19, 2015 | |
| 17. | Medical University of South Carolina, ” “Can E-Cigarettes Help Smokers Quit? Study Finds Smokers Who Are Willing to Use E-Cigarettes Tend to Smoke Less and Increase Their Quit Attempts,” sciencedaily.com, Dec. 29, 2017 | |
| 18. | D. Bush and M.L. Goniewicz, “A Pilot Study on Nicotine Residues in Houses of Electronic Cigarette Users, Tobacco Smokers, and Non-Users of Nicotine-Containing Products,” International Journal of Drug Policy, June 2015 | |
| 19. | Matthew L. Myers, “New U.S. Survey Shows Youth Cigarette Smoking Is at Record Lows, but E-Cigarettes and Cigars Threaten Progress,” tobaccofreekids.org, June 7, 2018 | |
| 20. | David Nutt, “Vaping Saves Lives. It’d Be Madness to Ban It,” theguardian.com, Oct. 14, 2016 | |
| 21. | Martin Dockrell, “Clearing up Some Myths Around E-Cigarettes,” publichealthmatters.blog.gov.uk, Feb. 20, 2018 | |
| 22. | Sally Satel, “How E-Cigarettes Could Save Lives,” washingtonpost.com, Feb. 14, 2014 | |
| 23. | Grover Norquist and Paul Blair, “Vaping for Tax Freedom,” nationalreview.com, Oct. 15, 2014 | |
| 24. | J. Scott Moody, “E-Cigarettes Poised to Save Medicaid Billions,” tobacco.ucsf.edu, Mar. 31, 2015 | |
| 25. | Grover Norquist, Lisa Nelson, Norm Singleton, et al., “Coalition Urges President Trump to Halt Regulatory Assault on Innovative Electronic Cigarette Industry,” atr.org, Feb. 4, 2019 | |
| 26. | Kaitlyn M. Berry, Jessica L. Fetterman, Emelia J. Benjamin, et al., “Association of Electronic Cigarette Use with Subsequent Initiation of Tobacco Cigarettes in US Youths,” JAMA Network Open, Feb. 1, 2019 | |
| 27. | American Lung Association, “E-cigarettes, ‘Vapes’ and JUULs: What Parents Should Know,” lung.org, Jan. 24, 2019 | |
| 28. | JUUL, “FAQS: JUULpod Basics,” support.juul.com (accessed Feb. 15, 2019) | |
| 29. | JUUL, “JUUL Savings Calculator,” juul.com (accessed Feb. 15, 2019) | |
| 30. | Maggie Fox, “Vaping, Juuling Are the New Smoking for High School Kids,” nbcnews.com, June 7, 2018 | |
| 31. | Dennis Thompson, “Vaping Tied to Rise in Stroke, Heart Attack Risk,” consumer.healthday.com, Jan. 30, 2019 | |
| 32. | Paul M. Ndunda and Tabitha M. Muutu, “9 – Electronic Cigarette Use Is Associated with a Higher Risk of Stroke,” abstractsonline.com, Feb. 6, 2019 | |
| 33. | Hanan Qasim Zubair, et al., “Short-Term E-Cigarette Exposure Increases the Risk of Thrombogenesis and Enhances Platelet Function in Mice,” Journal of the American Heart Association, Aug. 2018 | |
| 34. | Pablo Olmedo, et al., “Metal Concentrations in e-Cigarette Liquid and Aerosol Samples: The Contribution of Metallic Coils,” Environmental Health Perspectives, Feb. 21, 2018 | |
| 35. | Otmar Geiss, Ivana Bianchi, Josefa Barrero-Moreno, “Correlation of Volatile Carbonyl Yields Emitted by E-Cigarettes with the Temperature of the Heating Coil and the Perceived Sensorial Quality of the Generated Vapours,” International Journal of Hygiene and Environmental Health, May 2016 | |
| 36. | Matthew Rossheim, Melvin D. Livingston, Eric K. Soule, Helen A. Zeraye, and Dennis L. Thombs, “Electronic Cigarette Explosion and Burn Injuries, US Emergency Departments 2015–2017,” Tobacco Control, Sep. 2018 | |
| 37. | Mary Lee Clark, “Mason Report Finds E-Cigarette Explosions, Injuries Are More Common Than Previously Thought,” gmu.edu, Sep. 28, 2018 | |
| 38. | Rasha Ali, “E-Cigarette Battery Ignites Fire on American Airlines Flight from Las Vegas to Chicago,” usatoday.com, Jan. 6, 2019 | |
| 39. | David Williams, “A Man Dies After His E-Cigarette Explodes in His Face,” cnn.com, Feb. 5, 2019 | |
| 40. | Eli Rosenberg, “Exploding Vape Pen Caused Florida Man’s Death, Autopsy Says,” washingtonpost.com, May 17, 2018 | |
| 41. | Lawrence A. McKenna, Jr., “Electronic Cigarette Fires and Explosions in the United States 2009 – 2016,” usfa.fema.gov, July 2017 | |
| 42. | CDC, “About Electronic Cigarettes (E-Cigarettes),” cdc.gov, Nov. 29, 2018 | |
| 43. | FDA, “Vaporizers, E-Cigarettes, and Other Electronic Nicotine Delivery Systems (Ends),” fda.gov, Feb. 5, 2019 | |
| 44. | Blanca Myers, “What’s Inside Vape Juice?,” wired.co.uk, Apr. 25, 2017 | |
| 45. | Veppo, “What Is E-Juice or Vape Juice?,” veppocig.com (accessed Feb. 15, 2019) | |
| 46. | Richard Harris and Carmel Wroth, “FDA to Banish Flavored E-Cigarettes to Combat Youth Vaping,” npr.org, Sep. 11, 2019 | |
| 47. | CDC, “Outbreak of Lung Illness Associated with Using E-cigarette Products,” cdc.gov, Sep. 11, 2019 | |
| 48. | Lisa Rapaport, “Vaping May Aid Smoking Cessation but Also Boost Relapse Risk,” physiciansweekly.com, July 15, 2019 | |
| 49. | Virginia Langmaid, "FDA Chief Stays Mum on Plans for Banning Flavored Vapes," cnn.com, June 23, 2021 | |
| 50. | Grand View Research, "E-cigarette and Vape Market Size, Share & Trends Analysis Report by Distribution Channel (Online, Retail), by Product (Disposable, Rechargeable), by Component, by Region, and Segment Forecasts, 2021 - 2028," grandviewresearch.com, May 2021 | |
| 51. | Sheila Kaplan, "Juul Is Fighting to Keep Its E-Cigarettes on the U.S. Market," nytimes.com, July 5, 2021 | |
| 52. | Maria A. Villarroel, Amy E. Cha, and Anjel Vahratian, "Electronic Cigarette Use Among U.S. Adults, 2018," cdc.gov, Apr. 2020 | |
| 53. | CDC, "Youth and Tobacco Use," cdc.gov, Dec. 16, 2020 | |
| 54. | Megan Brenan, "Smoking and Vaping Remain Steady and Low in U.S.," gallup.com, Aug, 12, 2021 | |
| 55. | Janet Woodcock and Mitch Zeller, "FDA Makes Significant Progress in Science-Based Public Health Application Review, Taking Action on Over 90% of More Than 6.5 Million ‘Deemed’ New Tobacco Products Submitted," fda.gov, Sep. 9, 2021 | |
| 56. | Jacqueline Howard, "FDA Takes More Time to Decide on E-Cigarettes," cnn.com, Sep. 9, 2021 | |
| 57. | Mitch Zeller, "Perspective: FDA’s Preparations for the September 9 Submission Deadline," fda.gov, Aug. 31, 2020 | |
| 58. | Matt Richtel and Sheila Kaplan, "F.D.A. Authorizes E-Cigarettes to Stay on U.S. Market for the First Time," nytimes.com, Oct. 13, 2021 | |
| 59. | Vanessa Romo, "Marijuana Vaping among Teens Has More Than Doubled since 2013," npr.org, Oct. 25, 2021 | |
| 60. | Olufunmilayo H. Obisesan, Mohammadhassan Mirbolouk, and Albert D. Osei, "Association Between e-Cigarette Use and Depression in the Behavioral Risk Factor Surveillance System, 2016-2017," jamanetwork.com, Dec. 4, 2019 | |
| 61. | Carma Hassan, "FDA Orders Juul Labs to Remove Products from US Market," , June 23, 2022 | |
| 62. | Associated Press, "Juul Can Keep Selling Its Vaping Products in the U.S. — for Now,' , June 24, 2022 | |
| 63. | Christina Jewett, "Juul Settles Multistate Youth Vaping Inquiry for $438.5 Million," , Sep. 6, 2022 | |
| 64. | Michael Levenson, "F.D.A. Authorizes First Menthol-Flavored E-Cigarettes," nytimes.com, June 21, 2024 |
ProCon/Encyclopaedia Britannica, Inc. 325 N. LaSalle Street, Suite 200 Chicago, Illinois 60654 USA
Natalie Leppard Managing Editor [email protected]
© 2023 Encyclopaedia Britannica, Inc. All rights reserved
- Social Media
- Death Penalty
- School Uniforms
- Video Games
- Animal Testing
- Gun Control
- Banned Books
- Teachers’ Corner
Cite This Page
ProCon.org is the institutional or organization author for all ProCon.org pages. Proper citation depends on your preferred or required style manual. Below are the proper citations for this page according to four style manuals (in alphabetical order): the Modern Language Association Style Manual (MLA), the Chicago Manual of Style (Chicago), the Publication Manual of the American Psychological Association (APA), and Kate Turabian's A Manual for Writers of Term Papers, Theses, and Dissertations (Turabian). Here are the proper bibliographic citations for this page according to four style manuals (in alphabetical order):
[Editor's Note: The APA citation style requires double spacing within entries.]
[Editor’s Note: The MLA citation style requires double spacing within entries.]
Teen Vaping: The New Wave of Nicotine Addiction Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Over the years, the utilization of vaping products has dramatically increased, particularly among youth. With at least 12 deaths and close to 1,000 sickened, vaping, the enormously fashionable alternative for consuming nicotine or perhaps flavorful substances, has unexpectedly been riskier than predicted (Dinardo & Rome, 2019). The Centers for Disease Control (CDC) estimates that more than 2 million young people smoked e-cigarettes in 2021 (Dinardo & Rome, 2019).
It might have a significant effect if state officials asked the region’s health authority to ban all flavored vape goods in reaction to this issue to safeguard the youth’s well-being (Domenico et al., 2021). A state does have other options in addition to that. The best way to overcome this difficulty is for nations to incorporate free science-based application innovations. While enforcing an immediate ban benefits many parents, incorporating an app is preferable since it immediately communicates with the youth by showing them the negative impacts and ultimately nullifies any possibility of teenagers smoking.
Banning commodities, especially which bring some preconceived pleasures increases the demand for those who want them instead of cutting them. It is correct that banning vapes will have a slight effect as parents will majorly appreciate it, but it would only make the youth go to more extraordinary lengths seeking the vapes, hence imposing a threat more. This solution would work in the short term and involve many state officers and laws to force the action.
Alternatively, using scientifically constructed applications that are freely accessible in any state would have a significant positive effect as it directly communicates with youth. Showcasing the adverse effects of vaping and providing statistical facts in the form of notifications on youth’s phones will, by a majority, cut vape users as they are spoken to intellectually and emotionally. On the other hand, this would work over the long term, which is more profitable for the future generation and the nation’s government.
Therefore, incorporating a scientifically created application solution is the best overall solution and should be integrated into states where vaping is prone. A significant drop will be evident as soon as the government spreads awareness of the new freely accessible application. As many people work now not for themselves but the betterment of future generations, this solution would pose the best course of action in entirely eradicating vaping for the youth soon, with no possibility of newly developing again.
Dinardo, P., & Rome, E. S. (2019). Vaping: The new wave of Nicotine Addiction . Cleveland Clinic Journal of Medicine, 86 (12), 789–798. Web.
Domenico, L., DeRemer, C. E., Nichols, K. L., Campbell, C., Moreau, J. R., Childs, G. S., & Merlo, L. J. (2021). Combatting the epidemic of e-cigarette use and vaping among students and transitional-age youth. Current Psychopharmacology, 10 (1), 5–16. Web.
- The Epidemic of Opioid Addiction in the US
- Advocacy Programs to Address Disparities in Mental Health and Addiction Management
- Discussion: Vaping and E-Cigarettes
- Laws Regarding Vaping and E-Cigarettes
- The Vaping Ages 13 and Up
- Drug and Alcohol Abuse Among Teenagers
- Alcohol and Drug Abuse in Canada
- Misconceptions About Addiction
- Why Are Cigarettes Tightly Regulated?
- Episodes of The Business of Drugs Series
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2023, November 22). Teen Vaping: The New Wave of Nicotine Addiction. https://ivypanda.com/essays/teen-vaping-the-new-wave-of-nicotine-addiction/
"Teen Vaping: The New Wave of Nicotine Addiction." IvyPanda , 22 Nov. 2023, ivypanda.com/essays/teen-vaping-the-new-wave-of-nicotine-addiction/.
IvyPanda . (2023) 'Teen Vaping: The New Wave of Nicotine Addiction'. 22 November.
IvyPanda . 2023. "Teen Vaping: The New Wave of Nicotine Addiction." November 22, 2023. https://ivypanda.com/essays/teen-vaping-the-new-wave-of-nicotine-addiction/.
1. IvyPanda . "Teen Vaping: The New Wave of Nicotine Addiction." November 22, 2023. https://ivypanda.com/essays/teen-vaping-the-new-wave-of-nicotine-addiction/.
Bibliography
IvyPanda . "Teen Vaping: The New Wave of Nicotine Addiction." November 22, 2023. https://ivypanda.com/essays/teen-vaping-the-new-wave-of-nicotine-addiction/.
- Entertainment
- Environment
- Information Science and Technology
- Social Issues
Home Essay Samples Sociology Rogerian Argument
An Unbiased Overview on Vaping
*minimum deadline
Cite this Essay
To export a reference to this article please select a referencing style below

- Physical Appearance
- National Identity
- Caste System
Related Essays
Need writing help?
You can always rely on us no matter what type of paper you need
*No hidden charges
100% Unique Essays
Absolutely Confidential
Money Back Guarantee
By clicking “Send Essay”, you agree to our Terms of service and Privacy statement. We will occasionally send you account related emails
You can also get a UNIQUE essay on this or any other topic
Thank you! We’ll contact you as soon as possible.

Essay on Why Vaping Is Bad
Students are often asked to write an essay on Why Vaping Is Bad in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Why Vaping Is Bad
Health risks.
Vaping can cause serious health problems, including lung damage, heart disease, and cancer. The chemicals in e-cigarettes can damage the cells in your lungs, leading to inflammation and scarring. This can make it harder to breathe and increase your risk of infections.
Nicotine Addiction
E-cigarettes contain nicotine, which is addictive. Nicotine can harm your brain and body, leading to problems such as anxiety, depression, and addiction. It can also increase your risk of heart disease and cancer.
Secondhand Vapor
Vaping can release harmful chemicals into the air, which can be inhaled by people nearby. This is called secondhand vapor, and it can cause the same health problems as vaping.
Vaping is a dangerous habit that can have serious health consequences. If you are thinking about starting to vape, or if you are currently vaping, please reconsider. There are many other ways to enjoy yourself without putting your health at risk.
250 Words Essay on Why Vaping Is Bad
Risky experiment, liquid trouble.
E-cigarettes use a liquid that may contain nicotine, flavorings, and other chemicals. Nicotine is a drug that can harm brain growth in young people and can also cause addiction. The other chemicals in e-cigarettes could be bad for your lungs.
Lung Problems
Vaping can cause lung problems, such as scarring and inflammation. It can make you more likely to get infections. Some people have even died from vaping-related lung illnesses.
Not an Addiction-Curer
Vaping is often promoted as a way to quit smoking, but it isn’t a good idea. Vaping is not a proven way to quit smoking, and it can actually make it harder to quit.
Social Embarrassment
Vaping can also cause social problems. Some people find it annoying when others vape around them. It can also lead to arguments and conflicts.
Bad for Society
Vaping can be bad for the community as a whole. It can lead to more pollution and can make it harder for people to breathe.
Be Smart, Say No
500 words essay on why vaping is bad, health risks of vaping.
Vaping is inhaling and exhaling the vapor produced by an electronic cigarette or similar device. It is often promoted as a safer alternative to smoking, but there is no doubt that vaping has its own set of health risks. Some of the dangers associated with vaping include potential lung damage due to chemicals and metals entering the lungs, nicotine addiction, and the risk of burns or explosions due to faulty devices. The aerosol produced by e-cigarettes contains various chemicals, including formaldehyde, acetaldehyde, and acrolein, which can cause respiratory irritation and increase the risk of developing serious illnesses like cancer.
Addictive Nature of Nicotine
The majority of e-cigarettes contain nicotine, a highly addictive substance found in traditional cigarettes. Nicotine can adversely affect brain development, especially in young individuals whose brains are still developing. It has been linked to problems with memory, attention, and mood. Additionally, nicotine can increase the risk of heart disease, stroke, and cancer. E-cigarettes often deliver nicotine more efficiently than traditional cigarettes, leading to a quicker and stronger addiction.
Aerosol and Its Effects
In conclusion, there is ample evidence to suggest that vaping is not a safe alternative to smoking and is potentially harmful to our health. The aerosol produced by e-cigarettes contains harmful chemicals that can damage the lungs and pose a risk of addiction to nicotine. Until more research is conducted and the long-term effects of vaping are fully understood, it is best to avoid this practice and encourage others to do the same.
That’s it! I hope the essay helped you.
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Essay Service Examples Health Smoking
Essay on Why Is Vaping Bad
Table of contents
Vaping and the health risks behind it, introduction.
- Proper editing and formatting
- Free revision, title page, and bibliography
- Flexible prices and money-back guarantee
- Breland, Alison, et al. “Electronic Cigarettes: What Are They and What Do They Do?” Annals of the New York Academy of Sciences, vol. 1394, no. 1, 2016, pp.530.,doi:10.1111/nyas.12977.
- “E-Cigarettes: The Health Risks of Vaping.” NBCNews.com, NBCUniversal News Group, www.nbcnews.com/better/health/better-cigarettes-vaping-comes-its-own-set-health-risks-ncna819716.
- “Is Vaping Bad for You? Learn the Truth about the Side Effects Here.” Best Vape Deals - Cheap Vape Mods, Tanks & EJuice | Vaping Cheap, 10 Oct. 2018, vapingcheap.com/vaping-side-effects/.
- Palazzolo, and Dominic L. “Electronic Cigarettes and Vaping: A New Challenge in Clinical Medicine and Public Health. A Literature Review.” Frontiers, Frontiers, 1 Nov. 2013, www.frontiersin.org/articles/10.3389/fpubh.2013.00056/full.
- “The Different Types of Vapes You Need to Know.” Vaping360, vaping360.com/vaping-101/different-types-of-vapes/.
- “10 Shocking Dangers of Vaping | Health Risks Of Vaping And E-Cigarettes.” The Authentic Gay, 30 Jan. 2019, www.theauthenticgay.com/10-vaping-health-risks/
Our writers will provide you with an essay sample written from scratch: any topic, any deadline, any instructions.
Cite this paper
Related essay topics.
Get your paper done in as fast as 3 hours, 24/7.
Related articles

Most popular essays
- Adolescence
Adolescence is a time in someone’s life that can shape the future and who they are as a person....
This article determines the rates of concurrent use of nicotine and tobacco products among...
- Smoking Ban
Did you know smoking is one of the biggest contributors to illness and death in the uk? It is hard...
Over the years, smoking tobacco has remained one of the main factors in the increased levels of...
- Health Promotion
Promotion is a health strategy of the 21st century, which based on the new health perspective that...
The world has this consistent tendency to overlook women in many aspects unfortunately this...
The significance of the smoking cessation in the management of hypertension in a very vital and...
People do not understand exactly how dangerous vaping is to their bodies. Some believe it is...
Tobacco originated in the North and South American continents and became known by Europeans in the...
Join our 150k of happy users
- Get original paper written according to your instructions
- Save time for what matters most
Fair Use Policy
EduBirdie considers academic integrity to be the essential part of the learning process and does not support any violation of the academic standards. Should you have any questions regarding our Fair Use Policy or become aware of any violations, please do not hesitate to contact us via [email protected].
We are here 24/7 to write your paper in as fast as 3 hours.
Provide your email, and we'll send you this sample!
By providing your email, you agree to our Terms & Conditions and Privacy Policy .
Say goodbye to copy-pasting!
Get custom-crafted papers for you.
Enter your email, and we'll promptly send you the full essay. No need to copy piece by piece. It's in your inbox!
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012.

Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General.
1 introduction, summary, and conclusions.
- Introduction
Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation’s public and economic health in the future ( Perry et al. 1994 ; Kessler 1995 ). The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of American spending on health care ( Anderson 2010 ), is well-documented and undeniable. Although progress has been made since the first Surgeon General’s report on smoking and health in 1964 ( U.S. Department of Health, Education, and Welfare [USDHEW] 1964 ), nearly one in four high school seniors is a current smoker. Most young smokers become adult smokers. One-half of adult smokers die prematurely from tobacco-related diseases ( Fagerström 2002 ; Doll et al. 2004 ). Despite thousands of programs to reduce youth smoking and hundreds of thousands of media stories on the dangers of tobacco use, generation after generation continues to use these deadly products, and family after family continues to suffer the devastating consequences. Yet a robust science base exists on social, biological, and environmental factors that influence young people to use tobacco, the physiology of progression from experimentation to addiction, other health effects of tobacco use, the epidemiology of youth and young adult tobacco use, and evidence-based interventions that have proven effective at reducing both initiation and prevalence of tobacco use among young people. Those are precisely the issues examined in this report, which aims to support the application of this robust science base.
Nearly all tobacco use begins in childhood and adolescence ( U.S. Department of Health and Human Services [USDHHS] 1994 ). In all, 88% of adult smokers who smoke daily report that they started smoking by the age of 18 years (see Chapter 3 , “The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide”). This is a time in life of great vulnerability to social influences ( Steinberg 2004 ), such as those offered through the marketing of tobacco products and the modeling of smoking by attractive role models, as in movies ( Dalton et al. 2009 ), which have especially strong effects on the young. This is also a time in life of heightened sensitivity to normative influences: as tobacco use is less tolerated in public areas and there are fewer social or regular users of tobacco, use decreases among youth ( Alesci et al. 2003 ). And so, as we adults quit, we help protect our children.
Cigarettes are the only legal consumer products in the world that cause one-half of their long-term users to die prematurely ( Fagerström 2002 ; Doll et al. 2004 ). As this epidemic continues to take its toll in the United States, it is also increasing in low- and middle-income countries that are least able to afford the resulting health and economic consequences ( Peto and Lopez 2001 ; Reddy et al. 2006 ). It is past time to end this epidemic. To do so, primary prevention is required, for which our focus must be on youth and young adults. As noted in this report, we now have a set of proven tools and policies that can drastically lower youth initiation and use of tobacco products. Fully committing to using these tools and executing these policies consistently and aggressively is the most straight forward and effective to making future generations tobacco-free.
The 1994 Surgeon General’s Report
This Surgeon General’s report on tobacco is the second to focus solely on young people since these reports began in 1964. Its main purpose is to update the science of smoking among youth since the first comprehensive Surgeon General’s report on tobacco use by youth, Preventing Tobacco Use Among Young People , was published in 1994 ( USDHHS 1994 ). That report concluded that if young people can remain free of tobacco until 18 years of age, most will never start to smoke. The report documented the addiction process for young people and how the symptoms of addiction in youth are similar to those in adults. Tobacco was also presented as a gateway drug among young people, because its use generally precedes and increases the risk of using illicit drugs. Cigarette advertising and promotional activities were seen as a potent way to increase the risk of cigarette smoking among young people, while community-wide efforts were shown to have been successful in reducing tobacco use among youth. All of these conclusions remain important, relevant, and accurate, as documented in the current report, but there has been considerable research since 1994 that greatly expands our knowledge about tobacco use among youth, its prevention, and the dynamics of cessation among young people. Thus, there is a compelling need for the current report.
Tobacco Control Developments
Since 1994, multiple legal and scientific developments have altered the tobacco control environment and thus have affected smoking among youth. The states and the U.S. Department of Justice brought lawsuits against cigarette companies, with the result that many internal documents of the tobacco industry have been made public and have been analyzed and introduced into the science of tobacco control. Also, the 1998 Master Settlement Agreement with the tobacco companies resulted in the elimination of billboard and transit advertising as well as print advertising that directly targeted underage youth and limitations on the use of brand sponsorships ( National Association of Attorneys General [NAAG] 1998 ). This settlement also created the American Legacy Foundation, which implemented a nationwide antismoking campaign targeting youth. In 2009, the U.S. Congress passed a law that gave the U.S. Food and Drug Administration authority to regulate tobacco products in order to promote the public’s health ( Family Smoking Prevention and Tobacco Control Act 2009 ). Certain tobacco companies are now subject to regulations limiting their ability to market to young people. In addition, they have had to reimburse state governments (through agreements made with some states and the Master Settlement Agreement) for some health care costs. Due in part to these changes, there was a decrease in tobacco use among adults and among youth following the Master Settlement Agreement, which is documented in this current report.
Recent Surgeon General Reports Addressing Youth Issues
Other reports of the Surgeon General since 1994 have also included major conclusions that relate to tobacco use among youth ( Office of the Surgeon General 2010 ). In 1998, the report focused on tobacco use among U.S. racial/ethnic minority groups ( USDHHS 1998 ) and noted that cigarette smoking among Black and Hispanic youth increased in the 1990s following declines among all racial/ethnic groups in the 1980s; this was particularly notable among Black youth, and culturally appropriate interventions were suggested. In 2000, the report focused on reducing tobacco use ( USDHHS 2000b ). A major conclusion of that report was that school-based interventions, when implemented with community- and media-based activities, could reduce or postpone the onset of smoking among adolescents by 20–40%. That report also noted that effective regulation of tobacco advertising and promotional activities directed at young people would very likely reduce the prevalence and onset of smoking. In 2001, the Surgeon General’s report focused on women and smoking ( USDHHS 2001 ). Besides reinforcing much of what was discussed in earlier reports, this report documented that girls were more affected than boys by the desire to smoke for the purpose of weight control. Given the ongoing obesity epidemic ( Bonnie et al. 2007 ), the current report includes a more extensive review of research in this area.
The 2004 Surgeon General’s report on the health consequences of smoking ( USDHHS 2004 ) concluded that there is sufficient evidence to infer that a causal relationship exists between active smoking and (a) impaired lung growth during childhood and adolescence; (b) early onset of decline in lung function during late adolescence and early adulthood; (c) respiratory signs and symptoms in children and adolescents, including coughing, phlegm, wheezing, and dyspnea; and (d) asthma-related symptoms (e.g., wheezing) in childhood and adolescence. The 2004 Surgeon General’s report further provided evidence that cigarette smoking in young people is associated with the development of atherosclerosis.
The 2010 Surgeon General’s report on the biology of tobacco focused on the understanding of biological and behavioral mechanisms that might underlie the pathogenicity of tobacco smoke ( USDHHS 2010 ). Although there are no specific conclusions in that report regarding adolescent addiction, it does describe evidence indicating that adolescents can become dependent at even low levels of consumption. Two studies ( Adriani et al. 2003 ; Schochet et al. 2005 ) referenced in that report suggest that because the adolescent brain is still developing, it may be more susceptible and receptive to nicotine than the adult brain.
Scientific Reviews
Since 1994, several scientific reviews related to one or more aspects of tobacco use among youth have been undertaken that also serve as a foundation for the current report. The Institute of Medicine (IOM) ( Lynch and Bonnie 1994 ) released Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths, a report that provided policy recommendations based on research to that date. In 1998, IOM provided a white paper, Taking Action to Reduce Tobacco Use, on strategies to reduce the increasing prevalence (at that time) of smoking among young people and adults. More recently, IOM ( Bonnie et al. 2007 ) released a comprehensive report entitled Ending the Tobacco Problem: A Blueprint for the Nation . Although that report covered multiple potential approaches to tobacco control, not just those focused on youth, it characterized the overarching goal of reducing smoking as involving three distinct steps: “reducing the rate of initiation of smoking among youth (IOM [ Lynch and Bonnie] 1994 ), reducing involuntary tobacco smoke exposure ( National Research Council 1986 ), and helping people quit smoking” (p. 3). Thus, reducing onset was seen as one of the primary goals of tobacco control.
As part of USDHHS continuing efforts to assess the health of the nation, prevent disease, and promote health, the department released, in 2000, Healthy People 2010 and, in 2010, Healthy People 2020 ( USDHHS 2000a , 2011 ). Healthy People provides science-based, 10-year national objectives for improving the health of all Americans. For 3 decades, Healthy People has established benchmarks and monitored progress over time in order to encourage collaborations across sectors, guide individuals toward making informed health decisions, and measure the impact of prevention activities. Each iteration of Healthy People serves as the nation’s disease prevention and health promotion roadmap for the decade. Both Healthy People 2010 and Healthy People 2020 highlight “Tobacco Use” as one of the nation’s “Leading Health Indicators,” feature “Tobacco Use” as one of its topic areas, and identify specific measurable tobacco-related objectives and targets for the nation to strive for. Healthy People 2010 and Healthy People 2020 provide tobacco objectives based on the most current science and detailed population-based data to drive action, assess tobacco use among young people, and identify racial and ethnic disparities. Additionally, many of the Healthy People 2010 and 2020 tobacco objectives address reductions of tobacco use among youth and target decreases in tobacco advertising in venues most often influencing young people. A complete list of the healthy people 2020 objectives can be found on their Web site ( USDHHS 2011 ).
In addition, the National Cancer Institute (NCI) of the National Institutes of Health has published monographs pertinent to the topic of tobacco use among youth. In 2001, NCI published Monograph 14, Changing Adolescent Smoking Prevalence , which reviewed data on smoking among youth in the 1990s, highlighted important statewide intervention programs, presented data on the influence of marketing by the tobacco industry and the pricing of cigarettes, and examined differences in smoking by racial/ethnic subgroup ( NCI 2001 ). In 2008, NCI published Monograph 19, The Role of the Media in Promoting and Reducing Tobacco Use ( NCI 2008 ). Although young people were not the sole focus of this Monograph, the causal relationship between tobacco advertising and promotion and increased tobacco use, the impact on youth of depictions of smoking in movies, and the success of media campaigns in reducing youth tobacco use were highlighted as major conclusions of the report.
The Community Preventive Services Task Force (2011) provides evidence-based recommendations about community preventive services, programs, and policies on a range of topics including tobacco use prevention and cessation ( Task Force on Community Preventive Services 2001 , 2005 ). Evidence reviews addressing interventions to reduce tobacco use initiation and restricting minors’ access to tobacco products were cited and used to inform the reviews in the current report. The Cochrane Collaboration (2010) has also substantially contributed to the review literature on youth and tobacco use by producing relevant systematic assessments of health-related programs and interventions. Relevant to this Surgeon General’s report are Cochrane reviews on interventions using mass media ( Sowden 1998 ), community interventions to prevent smoking ( Sowden and Stead 2003 ), the effects of advertising and promotional activities on smoking among youth ( Lovato et al. 2003 , 2011 ), preventing tobacco sales to minors ( Stead and Lancaster 2005 ), school-based programs ( Thomas and Perara 2006 ), programs for young people to quit using tobacco ( Grimshaw and Stanton 2006 ), and family programs for preventing smoking by youth ( Thomas et al. 2007 ). These reviews have been cited throughout the current report when appropriate.
In summary, substantial new research has added to our knowledge and understanding of tobacco use and control as it relates to youth since the 1994 Surgeon General’s report, including updates and new data in subsequent Surgeon General’s reports, in IOM reports, in NCI Monographs, and in Cochrane Collaboration reviews, in addition to hundreds of peer-reviewed publications, book chapters, policy reports, and systematic reviews. Although this report is a follow-up to the 1994 report, other important reviews have been undertaken in the past 18 years and have served to fill the gap during an especially active and important time in research on tobacco control among youth.
- Focus of the Report
Young People
This report focuses on “young people.” In general, work was reviewed on the health consequences, epidemiology, etiology, reduction, and prevention of tobacco use for those in the young adolescent (11–14 years of age), adolescent (15–17 years of age), and young adult (18–25 years of age) age groups. When possible, an effort was made to be specific about the age group to which a particular analysis, study, or conclusion applies. Because hundreds of articles, books, and reports were reviewed, however, there are, unavoidably, inconsistencies in the terminology used. “Adolescents,” “children,” and “youth” are used mostly interchangeably throughout this report. In general, this group encompasses those 11–17 years of age, although “children” is a more general term that will include those younger than 11 years of age. Generally, those who are 18–25 years old are considered young adults (even though, developmentally, the period between 18–20 years of age is often labeled late adolescence), and those 26 years of age or older are considered adults.
In addition, it is important to note that the report is concerned with active smoking or use of smokeless tobacco on the part of the young person. The report does not consider young people’s exposure to secondhand smoke, also referred to as involuntary or passive smoking, which was discussed in the 2006 report of the Surgeon General ( USDHHS 2006 ). Additionally, the report does not discuss research on children younger than 11 years old; there is very little evidence of tobacco use in the United States by children younger than 11 years of age, and although there may be some predictors of later tobacco use in those younger years, the research on active tobacco use among youth has been focused on those 11 years of age and older.
Tobacco Use
Although cigarette smoking is the most common form of tobacco use in the United States, this report focuses on other forms as well, such as using smokeless tobacco (including chew and snuff) and smoking a product other than a cigarette, such as a pipe, cigar, or bidi (tobacco wrapped in tendu leaves). Because for young people the use of one form of tobacco has been associated with use of other tobacco products, it is particularly important to monitor all forms of tobacco use in this age group. The term “tobacco use” in this report indicates use of any tobacco product. When the word “smoking” is used alone, it refers to cigarette smoking.
- Organization of the Report
This chapter begins by providing a short synopsis of other reports that have addressed smoking among youth and, after listing the major conclusions of this report, will end by presenting conclusions specific to each chapter. Chapter 2 of this report (“The Health Consequences of Tobacco Use Among Young People”) focuses on the diseases caused by early tobacco use, the addiction process, the relation of body weight to smoking, respiratory and pulmonary problems associated with tobacco use, and cardiovascular effects. Chapter 3 (“The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide”) provides recent and long-term cross-sectional and longitudinal data on cigarette smoking, use of smokeless tobacco, and the use of other tobacco products by young people, by racial/ethnic group and gender, primarily in the United States, but including some worldwide data as well. Chapter 4 (“Social, Environmental, Cognitive, and Genetic Influences on the Use of Tobacco Among Youth”) identifies the primary risk factors associated with tobacco use among youth at four levels, including the larger social and physical environments, smaller social groups, cognitive factors, and genetics and neurobiology. Chapter 5 (“The Tobacco Industry’s Influences on the Use of Tobacco Among Youth”) includes data on marketing expenditures for the tobacco industry over time and by category, the effects of cigarette advertising and promotional activities on young people’s smoking, the effects of price and packaging on use, the use of the Internet and movies to market tobacco products, and an evaluation of efforts by the tobacco industry to prevent tobacco use among young people. Chapter 6 (“Efforts to Prevent and Reduce Tobacco Use Among Young People”) provides evidence on the effectiveness of family-based, clinic-based, and school-based programs, mass media campaigns, regulatory and legislative approaches, increased cigarette prices, and community and statewide efforts in the fight against tobacco use among youth. Chapter 7 (“A Vision for Ending the Tobacco Epidemic”) points to next steps in preventing and reducing tobacco use among young people.
- Preparation of the Report
This report of the Surgeon General was prepared by the Office on Smoking and Health (OSH), National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention (CDC), USDHHS. In 2008, 18 external independent scientists reviewed the 1994 report and suggested areas to be added and updated. These scientists also suggested chapter editors and a senior scientific editor, who were contacted by OSH. Each chapter editor named external scientists who could contribute, and 33 content experts prepared draft sections. The draft sections were consolidated into chapters by the chapter editors and then reviewed by the senior scientific editor, with technical editing performed by CDC. The chapters were sent individually to 34 peer reviewers who are experts in the areas covered and who reviewed the chapters for scientific accuracy and comprehensiveness. The entire manuscript was then sent to more than 25 external senior scientists who reviewed the science of the entire document. After each review cycle, the drafts were revised by the chapter and senior scientific editor on the basis of the experts’ comments. Subsequently, the report was reviewed by various agencies within USDHHS. Publication lags prevent up-to-the-minute inclusion of all recently published articles and data, and so some more recent publications may not be cited in this report.
- Evaluation of the Evidence
Since the first Surgeon General’s report in 1964 on smoking and health ( USDHEW 1964 ), major conclusions concerning the conditions and diseases caused by cigarette smoking and the use of smokeless tobacco have been based on explicit criteria for causal inference ( USDHHS 2004 ). Although a number of different criteria have been proposed for causal inference since the 1960s, this report focuses on the five commonly accepted criteria that were used in the original 1964 report and that are discussed in greater detail in the 2004 report on the health consequences of smoking ( USDHHS 2004 ). The five criteria refer to the examination of the association between two variables, such as a risk factor (e.g., smoking) and an outcome (e.g., lung cancer). Causal inference between these variables is based on (1) the consistency of the association across multiple studies; this is the persistent finding of an association in different persons, places, circumstances, and times; (2) the degree of the strength of association, that is, the magnitude and statistical significance of the association in multiple studies; (3) the specificity of the association to clearly demonstrate that tobacco use is robustly associated with the condition, even if tobacco use has multiple effects and multiple causes exist for the condition; (4) the temporal relationship of the association so that tobacco use precedes disease onset; and (5) the coherence of the association, that is, the argument that the association makes scientific sense, given data from other sources and understanding of biological and psychosocial mechanisms ( USDHHS 2004 ). Since the 2004 Surgeon General’s report, The Health Consequences of Smoking , a four-level hierarchy ( Table 1.1 ) has been used to assess the research data on associations discussed in these reports ( USDHHS 2004 ). In general, this assessment was done by the chapter editors and then reviewed as appropriate by peer reviewers, senior scientists, and the scientific editors. For a relationship to be considered sufficient to be characterized as causal, multiple studies over time provided evidence in support of each criteria.
Four-level hierarchy for classifying the strength of causal inferences based on available evidence.
When a causal association is presented in the chapter conclusions in this report, these four levels are used to describe the strength of the evidence of the association, from causal (1) to not causal (4). Within the report, other terms are used to discuss the evidence to date (i.e., mixed, limited, and equivocal evidence), which generally represent an inadequacy of data to inform a conclusion.
However, an assessment of a casual relationship is not utilized in presenting all of the report’s conclusions. The major conclusions are written to be important summary statements that are easily understood by those reading the report. Some conclusions, particularly those found in Chapter 3 (epidemiology), provide observations and data related to tobacco use among young people, and are generally not examinations of causal relationships. For those conclusions that are written using the hierarchy above, a careful and extensive review of the literature has been undertaken for this report, based on the accepted causal criteria ( USDHHS 2004 ). Evidence that was characterized as Level 1 or Level 2 was prioritized for inclusion as chapter conclusions.
In additional to causal inferences, statistical estimation and hypothesis testing of associations are presented. For example, confidence intervals have been added to the tables in the chapter on the epidemiology of youth tobacco use (see Chapter 3 ), and statistical testing has been conducted for that chapter when appropriate. The chapter on efforts to prevent tobacco use discusses the relative improvement in tobacco use rates when implementing one type of program (or policy) versus a control program. Statistical methods, including meta-analytic methods and longitudinal trajectory analyses, are also presented to ensure that the methods of evaluating data are up to date with the current cutting-edge research that has been reviewed. Regardless of the methods used to assess significance, the five causal criteria discussed above were applied in developing the conclusions of each chapter and the report.
- Major Conclusions
- Cigarette smoking by youth and young adults has immediate adverse health consequences, including addiction, and accelerates the development of chronic diseases across the full life course.
- Prevention efforts must focus on both adolescents and young adults because among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age.
- Advertising and promotional activities by tobacco companies have been shown to cause the onset and continuation of smoking among adolescents and young adults.
- After years of steady progress, declines in the use of tobacco by youth and young adults have slowed for cigarette smoking and stalled for smokeless tobacco use.
- Coordinated, multicomponent interventions that combine mass media campaigns, price increases including those that result from tax increases, school-based policies and programs, and statewide or community-wide changes in smoke-free policies and norms are effective in reducing the initiation, prevalence, and intensity of smoking among youth and young adults.
- Chapter Conclusions
The following are the conclusions presented in the substantive chapters of this report.
Chapter 2. The Health Consequences of Tobacco Use Among Young People
- The evidence is sufficient to conclude that there is a causal relationship between smoking and addiction to nicotine, beginning in adolescence and young adulthood.
- The evidence is suggestive but not sufficient to conclude that smoking contributes to future use of marijuana and other illicit drugs.
- The evidence is suggestive but not sufficient to conclude that smoking by adolescents and young adults is not associated with significant weight loss, contrary to young people’s beliefs.
- The evidence is sufficient to conclude that there is a causal relationship between active smoking and both reduced lung function and impaired lung growth during childhood and adolescence.
- The evidence is sufficient to conclude that there is a causal relationship between active smoking and wheezing severe enough to be diagnosed as asthma in susceptible child and adolescent populations.
- The evidence is sufficient to conclude that there is a causal relationship between smoking in adolescence and young adulthood and early abdominal aortic atherosclerosis in young adults.
- The evidence is suggestive but not sufficient to conclude that there is a causal relationship between smoking in adolescence and young adulthood and coronary artery atherosclerosis in adulthood.
Chapter 3. The Epidemiology of Tobacco Use Among Young People in the United States and Worldwide
- Among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age.
- Almost one in four high school seniors is a current (in the past 30 days) cigarette smoker, compared with one in three young adults and one in five adults. About 1 in 10 high school senior males is a current smokeless tobacco user, and about 1 in 5 high school senior males is a current cigar smoker.
- Among adolescents and young adults, cigarette smoking declined from the late 1990s, particularly after the Master Settlement Agreement in 1998. This decline has slowed in recent years, however.
- Significant disparities in tobacco use remain among young people nationwide. The prevalence of cigarette smoking is highest among American Indians and Alaska Natives, followed by Whites and Hispanics, and then Asians and Blacks. The prevalence of cigarette smoking is also highest among lower socioeconomic status youth.
- Use of smokeless tobacco and cigars declined in the late 1990s, but the declines appear to have stalled in the last 5 years. The latest data show the use of smokeless tobacco is increasing among White high school males, and cigar smoking may be increasing among Black high school females.
- Concurrent use of multiple tobacco products is prevalent among youth. Among those who use tobacco, nearly one-third of high school females and more than one-half of high school males report using more than one tobacco product in the last 30 days.
- Rates of tobacco use remain low among girls relative to boys in many developing countries, however, the gender gap between adolescent females and males is narrow in many countries around the globe.
Chapter 4. Social, Environmental, Cognitive, and Genetic Influences on the Use of Tobacco Among Youth
- Given their developmental stage, adolescents and young adults are uniquely susceptible to social and environmental influences to use tobacco.
- Socioeconomic factors and educational attainment influence the development of youth smoking behavior. The adolescents most likely to begin to use tobacco and progress to regular use are those who have lower academic achievement.
- The evidence is sufficient to conclude that there is a causal relationship between peer group social influences and the initiation and maintenance of smoking behaviors during adolescence.
- Affective processes play an important role in youth smoking behavior, with a strong association between youth smoking and negative affect.
- The evidence is suggestive that tobacco use is a heritable trait, more so for regular use than for onset. The expression of genetic risk for smoking among young people may be moderated by small-group and larger social-environmental factors.
Chapter 5. The Tobacco Industry’s Influences on the Use of Tobacco Among Youth
- In 2008, tobacco companies spent $9.94 billion on the marketing of cigarettes and $547 million on the marketing of smokeless tobacco. Spending on cigarette marketing is 48% higher than in 1998, the year of the Master Settlement Agreement. Expenditures for marketing smokeless tobacco are 277% higher than in 1998.
- Tobacco company expenditures have become increasingly concentrated on marketing efforts that reduce the prices of targeted tobacco products. Such expenditures accounted for approximately 84% of cigarette marketing and more than 77% of the marketing of smokeless tobacco products in 2008.
- The evidence is sufficient to conclude that there is a causal relationship between advertising and promotional efforts of the tobacco companies and the initiation and progression of tobacco use among young people.
- The evidence is suggestive but not sufficient to conclude that tobacco companies have changed the packaging and design of their products in ways that have increased these products’ appeal to adolescents and young adults.
- The tobacco companies’ activities and programs for the prevention of youth smoking have not demonstrated an impact on the initiation or prevalence of smoking among young people.
- The evidence is sufficient to conclude that there is a causal relationship between depictions of smoking in the movies and the initiation of smoking among young people.
Chapter 6. Efforts to Prevent and Reduce Tobacco Use Among Young People
- The evidence is sufficient to conclude that mass media campaigns, comprehensive community programs, and comprehensive statewide tobacco control programs can prevent the initiation of tobacco use and reduce its prevalence among youth.
- The evidence is sufficient to conclude that increases in cigarette prices reduce the initiation, prevalence, and intensity of smoking among youth and young adults.
- The evidence is sufficient to conclude that school-based programs with evidence of effectiveness, containing specific components, can produce at least short-term effects and reduce the prevalence of tobacco use among school-aged youth.
- Adriani W, Spijker S, Deroche-Gamonet V, Laviola G, Le Moal M, Smit AB, Piazza PV. Evidence for enhanced neurobehavioral vulnerability to nicotine during peri-adolescence in rats. Journal of Neuroscience. 2003; 23 (11):4712–6. [ PMC free article : PMC6740776 ] [ PubMed : 12805310 ]
- Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Preventive Medicine. 2003; 36 (3):272–81. [ PubMed : 12634018 ]
- Anderson G. Chronic Care: Making the Case for Ongoing Care. Princeton (NJ): Robert Wood Johnson Foundation; 2010. [accessed: November 30, 2011]. < http://www .rwjf.org/files /research/50968chronic .care.chartbook.pdf >.
- Bonnie RJ, Stratton K, Wallace RB, editors. Ending the Tobacco Problem: A Blueprint for the Nation. Washington: National Academies Press; 2007.
- Cochrane Collaboration. Home page. 2010. [accessed: November 30, 2010]. < http://www .cochrane.org/ >.
- Community Preventive Services Task Force. First Annual Report to Congress and to Agencies Related to the Work of the Task Force. Community Preventive Services Task Force. 2011. [accessed: January 9, 2012]. < http://www .thecommunityguide .org/library /ARC2011/congress-report-full.pdf >.
- Dalton MA, Beach ML, Adachi-Mejia AM, Longacre MR, Matzkin AL, Sargent JD, Heatherton TF, Titus-Ernstoff L. Early exposure to movie smoking predicts established smoking by older teens and young adults. Pediatrics. 2009; 123 (4):e551–e558. [ PMC free article : PMC2758519 ] [ PubMed : 19336346 ]
- Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ (British Medical Journal). 2004; 32 :1519. [ PMC free article : PMC437139 ] [ PubMed : 15213107 ] [ CrossRef ]
- Fagerström K. The epidemiology of smoking: health consequences and benefits of cessation. Drugs. 2002; 62 (Suppl 2):1–9. [ PubMed : 12109931 ]
- Family Smoking Prevention and Tobacco Control Act, Public Law 111-31, 123 U.S. Statutes at Large 1776 (2009)
- Grimshaw G, Stanton A. Tobacco cessation interventions for young people. Cochrane Database of Systematic Reviews. 2006;(4):CD003289. [ PubMed : 17054164 ] [ CrossRef ]
- Kessler DA. Nicotine addiction in young people. New England Journal of Medicine. 1995; 333 (3):186–9. [ PubMed : 7791824 ]
- Lovato C, Linn G, Stead LF, Best A. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database of Systematic Reviews. 2003;(4):CD003439. [ PubMed : 14583977 ] [ CrossRef ]
- Lovato C, Watts A, Stead LF. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database of Systematic Reviews. 2011;(10):CD003439. [ PMC free article : PMC7173757 ] [ PubMed : 21975739 ] [ CrossRef ]
- Lynch BS, Bonnie RJ, editors. Growing Up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington: National Academies Press; 1994. [ PubMed : 25144107 ]
- National Association of Attorneys General. Master Settlement Agreement. 1998. [accessed: June 9, 2011]. < http://www .naag.org/back-pages /naag/tobacco /msa/msa-pdf/MSA%20with %20Sig%20Pages%20and%20Exhibits .pdf/file_view >.
- National Cancer Institute. Changing Adolescent Smoking Prevalence. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2001. Smoking and Tobacco Control Monograph No. 14. NIH Publication. No. 02-5086.
- National Cancer Institute. The Role of the Media in Promoting and Reducing Tobacco Use. Bethesda (MD): U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2008. Tobacco Control Monograph No. 19. NIH Publication No. 07-6242.
- National Research Council. Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects. Washington: National Academy Press; 1986. [ PubMed : 25032469 ]
- Office of the Surgeon General Reports of the Surgeon General, U.S. Public Health Service. 2010. [accessed: November 30, 2010]. < http://www .surgeongeneral .gov/library/reports/index.html >.
- Perry CL, Eriksen M, Giovino G. Tobacco use: a pediatric epidemic [editorial] Tobacco Control. 1994; 3 (2):97–8.
- Peto R, Lopez AD. Future worldwide health effects of current smoking patterns. In: Koop CE, Pearson CE, Schwarz MR, editors. Critical Issues in Global Health. San Francisco: Wiley (Jossey-Bass); 2001. pp. 154–61.
- Reddy KS, Perry CL, Stigler MH, Arora M. Differences in tobacco use among young people in urban India by sex, socioeconomic status, age, and school grade: assessment of baseline survey data. Lancet. 2006; 367 (9510):589–94. [ PubMed : 16488802 ]
- Schochet TL, Kelley AE, Landry CF. Differential expression of arc mRNA and other plasticity-related genes induced by nicotine in adolescent rat forebrain. Neuroscience. 2005; 135 (1):285–97. [ PMC free article : PMC1599838 ] [ PubMed : 16084664 ]
- Sowden AJ. Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 1998;(4):CD001006. [ PubMed : 10796581 ] [ CrossRef ]
- Sowden AJ, Stead LF. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews. 2003;(1):CD001291. [ PubMed : 12535406 ] [ CrossRef ]
- Stead LF, Lancaster T. Interventions for preventing tobacco sales to minors. Cochrane Database of Systematic Reviews. 2005;(1):CD001497. [ PubMed : 15674880 ] [ CrossRef ]
- Steinberg L. Risk taking in adolescence: what changes, and why? Annals of the New York Academy of Sciences. 2004; 1021 :51–8. [ PubMed : 15251873 ]
- Task Force on Community Preventive Services. Recommendations regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. American Journal of Preventive Medicine. 2001; 20 (2 Suppl):S10–S15. [ PubMed : 11173214 ]
- Task Force on Community Preventive Services. Tobacco. In: Zaza S, Briss PA, Harris KW, editors. The Guide to Preventive Services: What Works to Promote Health? New York: Oxford University Press; 2005. pp. 3–79. < http://www .thecommunityguide .org/tobacco/Tobacco.pdf >.
- Thomas RE, Baker PRA, Lorenzetti D. Family-based programmes for preventing smoking by children and adolescents. Cochrane Database of Systematic Reviews. 2007;(1):CD004493. [ PubMed : 17253511 ] [ CrossRef ]
- Thomas RE, Perera R. School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews. 2006;(3):CD001293. [ PubMed : 16855966 ] [ CrossRef ]
- US Department of Health and Human Services. Preventing Tobacco Use Among Young People A Report of the Surgeon General. Atlanta (GA): US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994.
- US Department of Health and Human Services. Tobacco Use Among US Racial/Ethnic Minority Groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998.
- U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. 2nd ed. Washington: U.S. Government Printing Office; 2000.
- US Department of Health and Human Services. Reducing Tobacco Use: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000.
- US Department of Health and Human Services. Women and Smoking A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001.
- US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004.
- US Department of Health and Human Services. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. [ PubMed : 20669524 ]
- US Department of Health and Human Services. How Tobacco Smoke Causes Disease—The Biology and Behavioral Basis for Tobacco-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [ PubMed : 21452462 ]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. 2011. [accessed: November 1, 2011]. < http://www .healthypeople .gov/2020/default.aspx >.
- US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control; 1964. PHS Publication No. 1103.
- Cite this Page National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2012. 1, Introduction, Summary, and Conclusions.
- PDF version of this title (18M)
In this Page
Other titles in these collections.
- Reports of the Surgeon General
- Health Services/Technology Assessment Text (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Introduction, Summary, and Conclusions - Preventing Tobacco Use Among Youth and ... Introduction, Summary, and Conclusions - Preventing Tobacco Use Among Youth and Young Adults
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Home — Essay Samples — Social Issues — Vaping — Essay On Vaping
Essay on Vaping
- Categories: Vaping
About this sample

Words: 552 |
Published: Mar 5, 2024
Words: 552 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Social Issues

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 801 words
2 pages / 1085 words
1 pages / 540 words
2 pages / 1103 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Vaping
Vaping, once hailed as a safer alternative to traditional smoking, has now come under scrutiny due to its potential health risks and widespread usage among young people. This essay explores the various dangers associated with [...]
Vaping, the act of inhaling and exhaling aerosol produced by electronic cigarettes or vape pens, has become a subject of intense debate in recent years. Proponents argue that it offers several advantages over traditional [...]
Vapes, also known as e-cigarettes, or electronic are battery operated devices that people use to inhale an aerosol which typically contains nicotine , flavourings, and other types chemicals A vape is a handheld battery-powered [...]
Shmerling, R. (2019). Can vaping damage your lungs? What we do (and don’t) know. Harvard Health Publishing. Web.
In recent years, the rise of vaping among young people has sparked intense debate and controversy. As the popularity of e-cigarettes continues to grow, so do concerns about the potential health risks and societal implications [...]
Why is it important to people in same-sex relationships for gay marriage to be legalized? In the United States, there are only 14 states in which gay couples can marry. (Quin, Campbell) The truth is those who are homosexuals do [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Essays on Jews and Christians in late antiquity in honour of Oded Irshai
Andrew s. jacobs , harvard divinity school. [email protected].
[Authors and titles are listed at the end of this review.]
“The world of late antiquity” as a field of study since the 1970s is, perhaps, too often associated with a few specific Anglophone sites of elaboration and primarily with the intersections of early Christian studies (or, in another register, “patristics”) and post-Roman history (or, in another register, “classics”). The present volume, a Festschrift for Hebrew University professor Oded Irshai, is a salutary reminder that creative and generative thinking about late antiquity emerges from other, polyglot sites and can just as easily center Jews and Judaism alongside their Christian and “pagan” neighbors. Every contributor to the present volume (apart from co-editor and introduction author Martin Goodman) is a student, recent student, or faculty member in Israel and their offerings here traverse the same complicated grounds as the many works of Irshai himself: the social histories of religious contact, conflict, competition, and conquest in late antiquity, particularly among Jews and Christians, most notably in the fraught spaces of the “holy land.”
In an “ode to Oded” that opens the volume, Paula Fredriksen (who has co-written and co-taught with Irshai) explores Irshai’s “intellectual versatility,” engendered, in part, by a “late antiquicizing” postdoctorate year at Cambridge where he studied with, among others, Arnaldo Momigliano. Fredrisken then surveys three primary areas of Irshai’s vast publications (sacred violence, eschatology, and local real estate and power politics) before dwelling with real warmth on Irshai’s “intellectual generosity” (which I, too, have experienced during my career).
Following a brief introduction by Martin Goodman, who co-edited the volume with one of Irshai’s current doctoral students, the compact and uniformly smart set of essays unfolds in four uneven sections.
Three essays comprise the first section on “Religion and the Visual.” Yonatan Moss proposes a new solution to the riddle of the Helios mosaic found in Hammat Tiberias and other late ancient synagogues. Moss argues that the era of this mosaic’s construction was also one in which imperial imagery was uncoupled from its “pagan” associations with Sol Invictus and instead was seen as a secular echo of imperial imagery. On the one hand (a “minimalist” argument), this desacralization of the sun image made astrological representation more readily available to anti-idolatry mosaicists and synagogue heads. On the other hand (a “maximalist” argument) the de-divinized association between Constantinian emperors and sun imagery (as on coins) provided Jewish communities an opportunity to signal their affiliation with the imperial household, an opportunity that would become less available in the increasingly anti-Jewish fifth and sixth centuries.
Next, Noa Yuval-Hacham explores the brief emergence of a “hand of God” motif in Jewish art (a motif that would remain much more plentiful in Christian imagery of Late Antiquity). Beginning with the fulsome use of God’s hand in the paintings of the Dura Europos synagogue, Yuval-Hacham posits a Syrian origin for the motif, adopted by Jewish artists as it allowed them to find a representational “middle path between the hidden, formless God, and the God who is represented in human scale.” Yuval-Hacham then follows the path of the dual hands of God in the Dura scene of the parting of the Red Sea down various imagistic and interpretive byways of the fifth and sixth century.
In the final essay of this section, Zeev Weiss takes readers on a tour of late ancient Sepphoris, particularly its religious buildings (“a temple, two churches, and several synagogues”), with particular attention to how the Jews of Sepphoris might have lived in a typically multicultural urban space. While Moss’s essay in this section lacks any Helios images, Yuval-Hacham’s and Weiss’s essay each have several black-and-white images and reconstructions to help readers.
The longest section, on “Christian Perspectives,” comprises six essays. Yonatan Livneh revisits Cyril of Jerusalem’s promotion of his city’s interests; contra Jan Willem Drijvers’ argument that Cyril leveraged both the sacred sites of the city and its episcopal tradition stretching back to James, Livneh finds distinct reticence on the latter count, owing perhaps to rising anti-Judaism in the fourth century: “Jerusalem’s early history… remained a minefield.” Jacob Ashkenazi triangulates the efforts to establish a Christian capital between Juvenal, bishop of Jerusalem, and the empresses Eudocia and Pulcheria in the fifth century. Eudocia’s and Juvenal’s rival efforts in Jerusalem are placed in tension with Pulcheria’s efforts in Constantinople.
We move from episcopal politics to reinterpretations of sacred history. Osnat Rance (co-editor of the volume) gives a concise and persuasive summary of her argument to reassign the authorship and origins of an Encomium for the Martyrs found with other texts of Eusebius of Caesarea in a fifth-century Syriac manuscript. Per Rance, the particular sweep of martyrial history, from Old Testament martyrs to the third century CE, puts the text somewhere around Antioch after Eusebius’s death. In one of the more ambitious short offerings, Aryeh Kofsky and Serge Ruzer survey texts in Greek, Latin, and Syriac from Acts of the Apostles to the Cave of Treasures to trace diverse ideas about “Eschatological Ingathering of Israel in Early Christianity.” Oscillating between literal anticipation and spiritualized hesitation, this variety of texts from church orders to apocalypses to hagiographies index attitudes to Jews and Judaism among Christian thinkers.
Ora Limor brings her considerable expertise on relics and pilgrimage to the question of Jesus’s footprints at the Church of the Ascension, which began appearing in texts in Late Antiquity before being viewed by pilgrims, etched in stone, in the Middle Ages. Limor follows this trail from “text to texture”; what began as a marvel—footprints imprinted in sand that could never be wiped away—reported secondhand in literary texts in Rome and Gaul materialized as a stone monument centuries later witnessed by the pilgrims themselves. At issue, Limor suggests in her conclusion, may be internal Christian anxieties about divine embodiment as well as external competition, especially with Muslims, for proof of God’s ongoing presence in the holy land.
This section concludes with the most precise and focused of the essays: Daniel Schwartz’s correction of much modern interpretation of the verb ἐπηγάγετο in the Testimonium Flavianum as a pejorative reference to Jesus that might bolster the authenticity of the passage in question. Schwartz tracks this modern misinterpretation to a misreading of a parenthetical note in the nineteenth-century version of a sixteenth-century Greek lexicon. Nonetheless, Schwartz does not find in this correction an argument against the Testimonium ’s authenticity.
We turn to two essays from “Jewish Perspectives,” both of which assess Jewish (in both cases, rabbinic) views of Rome. Joshua Levinson plumbs the complexities of imperialized identity—through mimicry, magic, and diaspora refraction—in narratives of Palestinian rabbis sojourning in the Eternal City: “The journey to the heart of the other culture reveals that the very distinctions that enable identity are more unstable and porous than they may wish to acknowledge. Each side wears the other’s mask.” Levinson attempts a complex, even postcolonial read of rabbis considering Rome; Eyal Ben-Eliyahu’s aim is more concrete: to identify the two huts mentioned in rabbinic literature built by Romulus at the founding of the city in the actual landscape of late ancient Rome. Triangulating rabbinic and non-rabbinic evidence, Ben-Eliyahu lands on the “Casa Romuli” on the Palatine and Capitoline Hills.
The collection concludes with two essays on “Influence and Competition.” Hillel Newman brings us into the world of late ancient Jewish apocalypticism by placing the Sefer Eliyahu in literal dialogue (through juxtaposition of pertinent passages) with the Latin poet Commodian, particularly his apocalyptic Carmen de duo populis (which scholars date anywhere from the third through fifth centuries). Newman’s larger goal is to show that certain references to the apocalyptic “king from the East” may draw on common apocalyptic motifs dating long before the sixth century (he also adduces Lactantius to a lesser extent) and should not be taken as instances of vaticinia ex eventu that place the Sefer Eliyahu in a seventh-century context (Newman prefers the sixth century). The final essay, on “rest” in competitive Christian and Jewish contexts by Israel Jacob Yuval, comprises a vast sweep, both philosophical (“How did the idea of rest evolve?”) and historical, from Enūma Eliš to the Middle Ages, from Christian attempts to wrest rest from Saturday to Sunday to the deep—and perhaps very subtly anti-Christian—meditations of the Havdala liturgy.
Most of the essays are tightly focused on individual texts or images (or even on a single Greek word, in the case of Schwartz’s essay); only a few essays (by Kofsky and Ruzer, Limor, and Yuval) take a longer view of their subjects. They are all carefully argued and written (mistakes are few: a bishop’s death off by a decade, a passage ascribed to Genesis instead of Exodus) and they are refreshingly accessible, if not necessarily of immediate relevance, to all manner of students of late antiquity, no matter our particular specialization.
Readers will find that the essays cover a tremendous amount of ground, from divine imagery to ecclesiastical competition to pilgrimage to Jewish responses to empire. Should such a vast array of offerings seem too broad to those readers, it should be noted that these are topics all covered by Irshai himself, as the footnotes amply attest: as good Festschrifters , the authors here build on their honoree’s intellectual versatility and generosity.
Authors and Titles
PAULA FREDRIKSEN, with OSNAT RANCE — Ode to Oded
MARTIN GOODMAN — Introduction
Religion and the Visual
YONATAN MOSS — The Emperor’s New Clothes: the ‘Jewish Helios’ Enigma in its Christian Imperial Context
NOA YUVAL-HACHAM — Between Heaven and Earth: The Hand of God in Ancient Jewish Visuality
ZEEV WEISS — Shaping Religious Space: Pagans, Jews and Christians in Ancient Sepphoris
Christian Perspectives
YONATAN LIVNEH — Cyril’s New Jerusalem and His Omission of Local Church History
JACOB ASHKENAZI — Eudocia, Pulcheria, and Juvenal: Competition in the Field of Religion and the Built Environment of Jerusalem in the Fifth Century CE
OSNAT RANCE — ‘Although Their Names Escaped Me’: Local Patriotism and Saints Commemoration in Late Antique Syria
ARYEH KOFSKY and SERGE RUZER — Rethinking the Eschatological Ingathering of Israel in Early Christianity
ORA LIMOR — Divina Vestigia : Tracking the Early History of Jesus’ Footprints at the Mount of Olives
DANIEL R. SCHWARTZ — Reinach and Stephanus, Philo and Josephus: A Note on the Testimonium Flavianum
Jewish Perspectives
JOSHUA LEVINSON — When in Rome
EYAL BEN-ELIYAHU — Where were the Two Huts of Remus and Romulus in Rome?
Influence and Competition
HILLEL NEWMAN — The Hebrew Book of Elijah and Commodian’s Carmen de duobus populis
ISRAEL JACOB YUVAL — And the Rest is History: Sabbath versus Sunday

IMAGES
VIDEO
COMMENTS
Organization of the Report. This chapter presents a brief introduction to this report and includes its major conclusions followed by the conclusions of the chapters, the historical background of e-cigarettes, descriptions of the products, a review of the marketing and promotional activities of e-cigarette companies, and the current status of regulations from the U.S. Food and Drug ...
An updated Cochrane Review provides an independent, rigorous assessment of the best available evidence to date about electronic cigarettes for quitting smoking.. Scroll to the bottom of this article for a round-up of media coverage. The conclusions of this updated Review are unchanged since the last review was published two years ago: electronic cigarettes may help smokers stop their smoking ...
In conclusion, the debate surrounding vaping is complex and multifaceted, with valid arguments on both sides of the issue. While vaping may offer benefits as a harm reduction tool for adult smokers, the alarming rise in youth vaping poses a significant threat to public health. ... Argumentative Essay On Vaping. [online]. Available at: <https ...
There is moderate evidence for increased cough and wheeze in adolescents who use e-cigarettes and an association with e-cigarette use and an increase in asthma exacerbations. Conclusion 11-5. There is limited evidence of adverse effects of e-cigarette exposure on the respiratory system from animal and in vitro studies.
Conclusion: Weighing the Pros and Cons. Vaping is a complex issue with both advantages and disadvantages. While it has shown promise as a harm reduction tool for smokers and may contribute to reducing tobacco-related diseases, concerns about its health effects, especially among young people, cannot be ignored. ... An In-Depth Analysis Essay ...
This essay draws a startling parallel between the ingredients in vaping liquids and common household chemicals, revealing a dangerous truth. A Teen's Perspective: Join Jason, a high school student, as he shares his personal struggle with vaping addiction. His candid account gives voice to the hidden epidemic among young people and serves as a ...
An updated Cochrane Review, led by a University of Oxford researcher, provides an independent, rigorous assessment of the best available evidence to date about electronic cigarettes for quitting smoking. The conclusions of this updated Review are unchanged since the last review was published two years ago: electronic cigarettes may help smokers stop their smoking, and the
It causes 13% of all deaths, including from lung, mouth, throat and bladder cancer, emphysema, heart attack and stroke, to name just a few. People who smoke regularly and don't quit lose about ...
Smoking accounts for >16 million Americans living with chronic diseases. The chronic nature of smoking and vaping adverse effects on human health is addressed in this report. Through an in-depth exploration of the physiologic and psychological mechanisms involved, this report underscores the urgency of addressing the public health implications of these habits. The potential similarities ...
The topic of e-cigarettes is controversial. Opponents focus on e-cigarettes' risks for young people, while supporters emphasize the potential for e-cigarettes to assist smokers in quitting smoking. Most US health organizations, media coverage, and policymakers have focused primarily on risks to youths. Because of their messaging, much of the public—including most smokers—now consider e ...
Introduction. Use of electronic nicotine delivery systems (ENDS) (also called 'vaping'), particularly electronic cigarettes (e-cigarettes), has increased rapidly in many high-income countries since about 2010, especially among youths and young adults. 1 2 As an e-cigarette contains fewer of the toxic and carcinogenic chemicals that are in a conventional cigarette, e-cigarette use is ...
The origins of vaping. Vaping achieved widespread popularity over the past decade, but its origins date back almost a century and are summarized in figure 1.The first known patent for an "electric vaporizer" was granted in 1930, intended for aerosolizing medicinal compounds.23 Subsequent patents and prototypes never made it to market,24 and it wasn't until 1979 that the first vape pen ...
Vaping has numerous devastating effects and did not worth doing. Preview of main points. There are two major reasons to give up a habitude of vape. Firstly, vaping is addictive and undermines the ability to self-control. Secondly, usage of a vape, even if it is nicotine-free, poses a health hazard and leads to diseases of the respiratory system.
E-cigarettes help adults quit smoking and lowers youth smoking rates. A July 2019 study found that cigarettes smokers who picked up vaping were 67% more likely to quit smoking. A New England Journal of Medicine study found that e-cigarettes are twice as effective at getting people to quit smoking as traditional nicotine replacements such as the ...
Get a custom essay on Teen Vaping: The New Wave of Nicotine Addiction. It might have a significant effect if state officials asked the region's health authority to ban all flavored vape goods in reaction to this issue to safeguard the youth's well-being (Domenico et al., 2021). A state does have other options in addition to that.
In conclusion, smokers who quit by switching to regular electronic cigarettes or vaping can reduce risk and reverse harm from nicotine smoking. ... The writer attempts a Rogerian approach, seeking common ground between supporters and critics of vaping. The essay covers multiple perspectives and sources, providing some insight into the ...
Conclusion: A Call for Awareness and Regulation. Vaping, once seen as a promising alternative to traditional smoking, has revealed a host of dangers, especially for young users. ... Argumentative Essay On Vaping Essay. In recent years, the rise of vaping among young people has sparked intense debate and controversy. As the popularity of e ...
Students are often asked to write an essay on Vaping in their schools and colleges. And if you're also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic. ... Conclusion. In conclusion, while vaping is often perceived as a safer alternative to traditional smoking, it is not without risks. The potential ...
Conclusion. Vaping is a dangerous habit that can have serious health consequences. If you are thinking about starting to vape, or if you are currently vaping, please reconsider. ... 500 Words Essay on Why Vaping Is Bad Health Risks of Vaping. Vaping is inhaling and exhaling the vapor produced by an electronic cigarette or similar device. It is ...
Conclusion. In conclusion, vaping is a topic of significant importance due to its potential health risks and the marketing tactics of the vaping industry. While some people argue that vaping is a safer alternative to smoking, and can help smokers quit, the potential health risks should not be ignored. Governments need to implement further ...
Essay On Vaping. Vaping has become a staple of today's culture. From young teens getting into "mods" and adults transitioning into e-cigarettes in an attempt to lead a healthier lifestyle. Most people would like to believe that this "Vaping" trend is sign that cigarettes are about to become outdated, and that people are switching to a ...
Introduction. People say all the time that vaping is not as bad as smoking cigarettes but vaping still doesn't prevent health problems. Vaping can still cause problems such as popcorn lungs, and popcorn lungs can lead to death. There is a certain chemical that can cause popcorn lungs and it is called diacetyl, and it is in these vaping ...
Anti-Vaping essay (How vaping causes harm, a school assignment) Vaping has been significantly grown in popularity throughout the years after it was first introduced. Lots of people have hopped on this harmful trend, and yes- that's a problem. Even though it might seem safe, the use of E-cigarettes does not help you quit tobacco products, they ...
Tobacco use is a global epidemic among young people. As with adults, it poses a serious health threat to youth and young adults in the United States and has significant implications for this nation's public and economic health in the future (Perry et al. 1994; Kessler 1995). The impact of cigarette smoking and other tobacco use on chronic disease, which accounts for 75% of American spending ...
Vaping. Vaping has become a popular trend in recent years, especially among young adults and teenagers. This essay will explore the history of vaping, the debates surrounding its use, and how these debates have evolved over time. By examining the development of the topic, we can better understand the current state of vaping and its implications ...
[Authors and titles are listed at the end of this review.] "The world of late antiquity" as a field of study since the 1970s is, perhaps, too often associated with a few specific Anglophone sites of elaboration and primarily with the intersections of early Christian studies (or, in another register, "patristics") and post-Roman history (or, in another register, "classics"). The ...